June 26, 2020 — Abbott announced new data from the company's LightLab Initiative that showed optical coherence tomography (OCT) imaging significantly changes how physicians decide to treat a vessel compared to traditional angiography by providing physicians improved visualization within a patient's blood vessels. Data from the study revealed physicians altered their treatment strategy in 88 percent of coronary artery blockages based on new information provided by OCT.
"After planning a procedure with angiography alone, we exposed physicians to all the information provided by OCT on the same blockage and were able to demonstrate the significant impact that the information had on our decisions," said Hiram Bezerra, M.D., professor of medicine at the University of South Tampa and the director of cardiac interventional services at Tampa General Hospital in Florida. "OCT takes the guesswork out of angiography, offering doctors real-time high-quality granularity and precision when performing PCIs, and helping doctors make real-time decisions in the cath lab."
This is the first data release from Abbott's LightLab Initiative, which was presented as part of a virtual three-day PCR e-Course held by the European Association of Percutaneous Cardiovascular Interventions (EAPCI), June 25-27. The new data provides strong evidence of the value of using OCT for decision-making within the PCI procedure. Initial data found:
• OCT changes angiographic-based decisions in 88% of lesions.
• After deploying a stent, physicians made changes in treating 31% of lesions based on OCT information to treat damage to the artery previously invisible with angiography alone.
• Physicians improved their assessment of potential blockages as a result of using OCT, which better helped inform which size of stent to use and optimal stent deployment compared with angiography alone.
"The LightLab Initiative has given us great insights into the challenges facing interventional cardiologists in the cath lab and the impact OCT can have on the decisions physicians make in treating their patients," said Nick West, M.D., divisional vice president, medical affairs, and chief medical officer of Abbott's vascular business. "The data has also highlighted how effective OCT can be at treating patients with complex cardiovascular disease with greater precision."
Abbott Vascular LightLab Initiative
The LightLab Initiative was designed to examine the role and impact of OCT on physician decision-making, procedural efficiency and procedural safety over angiography during procedures for patients with vascular disease. Abbott field clinical engineers collaborated with interventional cardiologists in 12 medical centers across the United States and collected PCI procedural data over a 12-month period.
Of the 2,203 procedures and 1,016 interventions that were assessed in the first phase of the LightLab Initiative, doctors used OCT before and after stenting in 652 lesions.
The level of detail and the volume of data collected in this real-world patient cohort demonstrates a clear and important impact of OCT on lesion assessment, procedural planning and stent optimization, with further analyses from subsequent phases of the program planned in coming months. The subsequent phases of the LightLab Initiative will focus on optimizing the prescribed treatment steps when using OCT to achieve greater efficiency (shorter timing) and safety (lower contrast and radiation exposure) gains, thereby identifying and removing barriers to OCT adoption.
About Optical Coherence Tomography
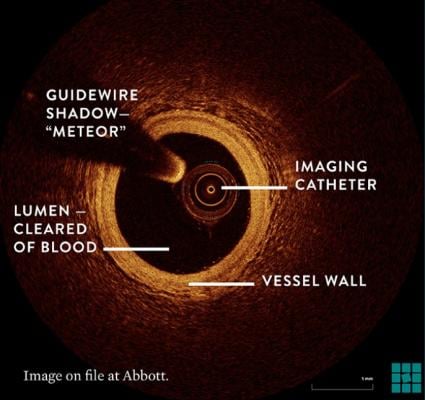
Imaging techniques such as OCT have been shown to improve outcomes during stenting procedures,[1] but remain underutilized. OCT is an intracoronary imaging platform that uses light-based technology to help characterize and assess coronary arteries from inside the vessel with high precision, allowing for assessment of the degree and characteristics of coronary artery disease, accurate dimensional measurement of the artery and assessment of the quality of stent deployment.[2]
Using laser technology, OCT captures high-resolution images inside a patient's arteries, displaying the type and severity of disease in the vessel, as well as enabling more accurate measurements to determine how the patient should be treated.
For more information: www.abbott.com
References:


 January 28, 2026
January 28, 2026 









