Most people assume strokes only happen to octogenarians, but recent evidence suggests that survivors of childhood cancer have a high risk of suffering a stroke at a surprisingly young age.
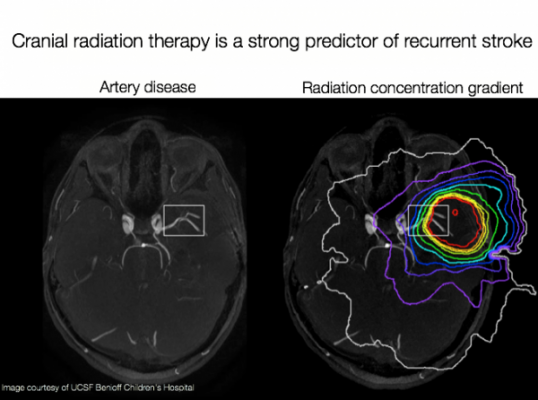
A new study from the UC San Francisco Pediatric Brain Center shows that childhood cancer survivors suffering one stroke have double the risk of suffering a second stroke, when compared with non-cancer stroke survivors. The study found that the main predictors of recurrent stroke were cranial radiation therapy, hypertension and older age at first stroke – factors that could help physicians identify high-risk patients.
The findings provide strong evidence for adjusting secondary stroke prevention strategies in these patients, and to aggressively detect and treat modifiable stroke risk factors, such as hypertension. Findings appear in the Aug. 26, 2015, online issue of Neurology, the medical journal of the American Academy of Neurology.
“We are at a point where more children are surviving cancer because of life-saving interventions,” said Sabine Mueller, M.D., Ph.D., director of the UCSF Pediatric Brain Tumor Center in UCSF Benioff Children’s Hospital San Francisco and co-author of the study. “ Now, we are facing long-term problems associated with these interventions.”
The Pediatric Brain Center (PBC) is a collaboration between two UCSF centers — the Pediatric Brain Tumor Center, and Pediatric Stroke and Cerebrovascular Disease Center — that brings specialists together to provide coordinated care for patients, while conducting research to better understand how to care for children.
The researchers analyzed retrospective data from the Childhood Cancer Survivor Study (CCSS), which has followed 14,358 survivors diagnosed between 1970 and 1986 in the United States and Canada to track long-term outcomes of cancer treatment. All of the recruits were diagnosed with cancer before age 21. To assess stroke recurrence rates, the researchers sent a second survey to participants who had reported a first stroke, asking them to confirm their first stroke and report if and when they had had another. The researchers analyzed the respondent demographics and cancer treatments to identify any potential predictors of recurrent strokes.
Of the 271 respondents who reported having had a stroke, 70 also reported a second one. Overall, the rate of recurrence within the first 10 years after an initial stroke was 21 percent, which is double the rate of the general population of stroke survivors. The rate was even higher — 33 percent — for patients who had received cranial radiation therapy.
Previous research has shown that radiation therapy targeting the head is a strong predictor of a first stroke. In an earlier study, the authors found that children treated for brain tumors were 30 times more likely to suffer a stroke compared to their siblings. While the exact mechanisms are unclear, the scientists think high-dose radiation causes the blood vessels to constrict and encourage blockage.
“If they have one stroke, it’s not actually surprising that they have a high risk of getting another stroke,” said Heather Fullerton, M.D., professor of neurology, founder of the UCSF Pediatric Stroke and Cerebrovascular Disease Center, and first author of the study. “You might use aspirin after the first stroke to try to reduce blood clots, but you’re not making those diseased blood vessels go away.”
The findings have significant implications for medical follow-up in childhood cancer patients. The authors said that current survivor screening guidelines do not recommend checking for diseased blood vessels, even though the signs are visible in standard MRIs.
“The radiologists are so focused on looking in the brain area where the tumor used to be that they’re not looking at the blood vessels,” Fullerton said.
Based on the findings, UCSF has updated protocols for monitoring patients to include screening for both blood vessel injury and modifiable stroke risk factors, but it is not required on a national level.
“If we could identify high-risk patients, we could recommend they be followed by a pediatric stroke specialist,” said Mueller. “That will be huge in providing effective follow-up care for these children.”
Other collaborators on the study are Robert R. Goldsby, M.D., professor of pediatrics and director of the UCSF Survivors of Childhood Cancer Program; Kayla Stratton, MS, and Wendy Leisenring, Sc.D., of the Fred Hutchinson Cancer Research Center; Gregory Armstrong, M.D., Leslie Robinson, Ph.D., and Kevin Krull, Ph.D., of St. Jude’s Children’s Research Hospital; Marilyn Stovall, Ph.D., and RE Weathers, MS, of the University of Texas, and Charles Sklar, Ph.D., of Memorial Sloan-Kettering Cancer Center.
This work was supported by the National Cancer Institute (U24 CA 55727), the Cancer Center Support (CORE), the American Lebanese-Syrian Associated Charities, the National Center for Advancing Translational Sciences, the Frank A. Campini Foundation and a private donation from the LaRoche family.
UCSF Benioff Children’s Hospital San Francisco is the only California state-designated children’s medical center in San Francisco. The hospital is one of the leading children's hospitals in the nation, according to U.S. News & World Report. Its expertise covers virtually all pediatric conditions, including cancer, heart disease, neurological disorders, organ transplants and orthopedics as well as the care of critically ill newborns.
For more information: www.ucsf.edu/news.


 February 02, 2026
February 02, 2026