
A heart failure patient wearing the SensiVest remote monitoring system for a two-minute a day assessment.
July 13, 2017 — About 5.7 million adults in the U.S. suffer from heart failure, and because of a dangerous buildup of fluid in their lungs, more than half of those patients end up back in the hospital within six months. But researchers say a high-tech vest that is entering U.S. trials may help doctors monitor a heart patient’s symptoms remotely, which may prevent the need for rehospitalization.
The SMILE Trial (Sensible Medical Innovations Lung fLuid status monitor allows rEducing readmission rate of heart failure patients study) will look at the efficacy of the SensiVest, a product developed by Sensible Medical Innovations, headquartered in Israel. The system is comprised of a wearable vest containing two embedded sensors, one in front and one behind the patient, and a bedside console.
“The major cause of readmission for heart failure patients is excess fluid in the lungs,” said William Abraham, M.D., FACC, director of the Division of Cardiovascular Medicine at The Ohio State University Wexner Medical Center, who is leading a randomized, clinical trial of the vest. “The vest allows us to see when the lungs are trending toward being too wet so a patient’s medication can be adjusted before they even notice any symptoms.”
Watch a VIDEO showing how the vest works and to hear more about it from Abraham.
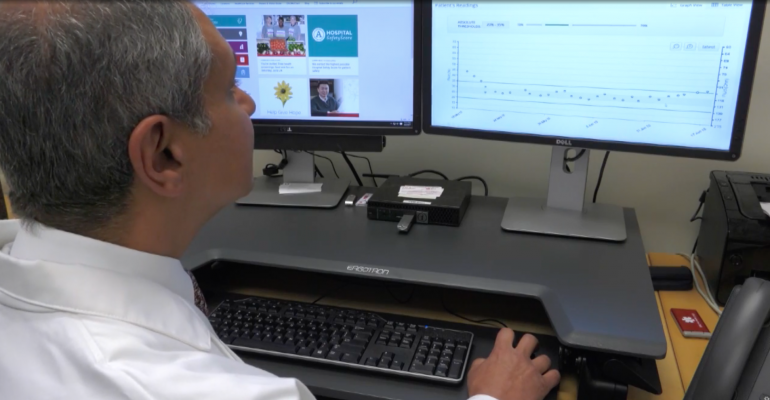
The vest uses radar technology to “see through” the chest and accurately detect the amount of fluid in the lungs. A patient wears the vest for just 90 seconds a day and the information collected is automatically uploaded to a cloud server. The patient’s cardiologist can review the data to determine if any treatment adjustments need to be made to restore the lungs to healthy fluid levels.
“This technology gives us absolute and actionable data of lung fluid content that we can use to keep patients healthy and out of the hospital,” Abraham said. “The fact that it is completely non-invasive and takes less than two minutes a day to use, allows patients to live a better quality of life with heart failure.”
A study initially conducted in Israel reported that hospital readmission rates were reduced by 87 percent for patients who were part of the study.
The vest uses the same technology used by the military for things like “seeing through” walls before entering a building or searching through rubble for survivors after a natural disaster.


 February 03, 2026
February 03, 2026 









