October 18, 2017 — The U.S. Food and Drug Administration (FDA) recently approved a new treatment option for patients who have been diagnosed with moderate to severe central sleep apnea (CSA). The Respicardia Remedē System is an implantable pacemaker-like device that stimulates the phrenic nerve located in the chest that is responsible for sending signals to the diaphragm to stimulate breathing.
Watch a VIDEO showing a demonstration of how the Remede System works.
“This implantable device offers patients another treatment option for central sleep apnea,” said Tina Kiang, Ph.D., acting director of the Division of Anesthesiology, General Hospital, Respiratory, Infection Control and Dental Devices in the FDA’s Center for Devices and Radiological Health. “Patients should speak with their healthcare providers about the benefits and risks of this new treatment compared to other available treatments.”
Sleep apnea is a disorder that causes individuals to have one or more pauses in breathing or shallow breaths during sleep. Breathing pauses can last from a few seconds to minutes. Central sleep apnea occurs when the brain fails to send signals to the diaphragm to breathe, causing an individual to stop breathing during sleep for a period of 10 seconds or more before restarting again. According to the National Institute of Health’s National Center on Sleep Disorders Research, central sleep apnea can lead to poor sleep quality and may result in serious health issues, including an increased risk for high blood pressure, heart attack, heart failure, stroke, obesity, and diabetes. Common treatment options for moderate to severe sleep apnea include medication, positive airway pressure devices, or surgery.
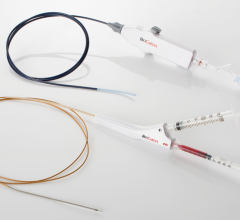
The Remedē System is comprised of a battery pack surgically placed under the skin in the upper chest area and small, thin wires that are inserted into the blood vessels in the chest near the nerve (phrenic) that stimulates breathing. The system monitors the patient’s respiratory signals during sleep and stimulates the nerve to move the diaphragm and restore normal breathing.
The FDA evaluated data from 141 patients to assess the effectiveness of the Remedē System in reducing apnea hypopnea index (AHI), a measure of the frequency and severity of apnea episodes. After six months, AHI was reduced by 50 percent or more in 51 percent of patients with an active Remedē System implanted. AHI was reduced by 11 percent in patients without an active Remedē System implanted.
The FDA said the most common adverse events reported included concomitant device interaction, implant site infection and swelling, and local tissue damage or pocket erosion. The Remedē System should not be used by patients with an active infection or by patients who are known to require magnetic resonance imaging. This device is not intended for use in patients with obstructive sleep apnea, a condition in which the patient attempts to breathe, but the upper airway is partially or completely blocked.
Use of the Remede Device in Heart Failure Patients
The Remede device is being investigated in trials for possible use to treat heart failure patients with CSA. In September, the Lancet published results from an international, randomized study showing how the device significantly improves symptoms in patents with CSA, without causing serious side effects. William Abraham, M.D., co-lead author and director of the Division of Cardiovascular Medicine at The Ohio State University Wexner Medical Center, presented findings from the study at the 2017 European Society of Cardiology (ESC) congress.
Review the study in the Lancet.
Unlike the more common obstructive sleep apnea, in which the airway partially collapses and causes pauses in breathing, CSA occurs when the brain fails to control breathing during sleep. “CSA is a serious concern because it affects about a third of people with heart failure and it’s known to make the condition worse,” Abraham said.
“Currently, we don’t have good treatments available. Positive airway pressure devices have been used, but many patients don’t tolerate them well and a recent study showed them to be harmful.”
The study used the Respicardia Remede System, which is a pacemaker-like device designed to improve cardiovascular health by restoring natural breathing during sleep in patients with CSA.
Abraham, along with lead author Maria Rosa Costanzo, M.D., at Advocate Heart Institute in Naperville, Ill., led the study at 31 hospitals in the United States, Germany and Poland. The research team tested the safety and effectiveness of a transvenous phrenic nerve stimulator. Much like a pacemaker, it sends a regular signal telling the diaphragm to breathe during sleep.
In the randomized study, 151 patients were implanted with the device. Ten were excluded due to non-study related medical issues or deaths, exiting the study or missing visits. During the first six months of evaluation, 68 devices were activated for treatment, while 73 were left inactive as the control group. Between six and 12 months of follow-up, all patients received the neurostimulation treatment.
At the six month evaluation, the device reduced CSA events per hour by half or more for 35 of the 68 members (51 percent) of the treatment group. Only eight (11 percent) of those in the control group achieved the same reduction. Other important sleep measures, such as the amount of time spent with a low blood oxygen level, were also significantly improved. About a third of patients in the treatment group reported therapy-related discomfort that was resolved with some reprogramming of the device.
“Not only did we see this reduction in events per hour, the patients also rated themselves better on the Epworth Sleepiness Scale (meaning they were less sleepy during the day) and on a global assessment of their overall quality of life,” Abraham said. “This tells us the effects of neurostimulation are clinically relevant and this could be a promising therapy for those with central sleep apnea.”
Watch a VIDEO showing a demonstration of how the Remede System works.

 January 29, 2026
January 29, 2026