COVID-19 has posed challenges for physicians whose cardiac patients are at-risk and reluctant to schedule an office visit. Floyd Russak, M.D., of Russak Personalized Medicine, an internal medicine physician practicing in Greenwood Village, Colo., manages many cardiac patients who do not have ready access to a cardiologist. “More people are afraid of going to the doctor now when they have cardiac issues,” he said. “They’re concerned about COVID, but in their caution, they can die from an unmonitored, untreated cardiac condition. In fact, more people currently die each day from cardiac disease than from COVID.”1
Russak noted he has seen more atrial fibrillation (AFib) since COVID-19. He attributes some of that as being due to people’s anxiety about the virus; some AFib, he noted, is doubtlessly related to increases in lung disease. Yet at a time when cardiac monitoring is more critically important than ever, patients may have greater reluctance to schedule an appointment.
Cardiologist Dwayne Schmidt, M.D., of Cardiovascular Health Clinic in Oklahoma City, added, “Patients are definitely more guarded about going to large medical facilities. COVID has probably reduced office visits by 20 percent. Yet if a patient wearing a traditional Holter monitor does not come into the office, that’s a problem. We now have new wearable ECG solutions that make it simpler both for the patient and the clinician and can be administered via telehealth.”
The Unique Needs of Rural Populations
Patients who live in rural areas face the additional challenge of having to commute to the doctor. Russak, who sees patients from remote areas around Pitkin County, Colo., said, “Rural populations often don’t have access to a cardiologist at all. Internists have to get extra training and consult with cardiologists by phone.” Applying a traditional Holter monitor is something internists serving a rural patient population must learn to do themselves; it cannot be done by medical assistants. In addition, traditional Holter monitors may collect only a limited amount of data, require the patient to be in-office for application and then return a day or two to have it adjusted, removed, and read. Lastly, a Holter monitor may have numerous wires that can make it uncomfortable to wear for the patient. All the above adds additional complexity to the process.
Rural clinics covering large geographies may have a limited number of monitors, resulting in patient wait lists. Once a Holter monitor cycle is complete, data is sent to a third party for analysis. Results can take weeks and delay diagnosis and treatment. If the monitoring cycle does not capture irregularities and patient symptoms persist, the patient may need to repeat the entire monitoring process.
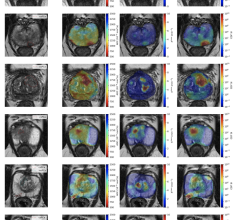
Fortunately, there are next-generation wearable devices like the Cardea SOLO ECG System that make this process much more convenient for the rural patient and the physician alike. These are small, compact sensors that are water-resistant and lightweight, allowing patients greater freedom to carry on with their normal activities while wearing them. Schmidt said that the data from them is comparable to that from a traditional Holter monitor.
These devices collect data for a longer period of time than a Holter monitor — typically about a week’s worth. That provides more information and does not require back-to-back commutes to the doctor’s office, which is particularly inconvenient for patients who live some distance away. Russak encourages his patients to make notes when they experience symptoms; this information then can be synced up with the report from the wearable device. “The ECG data is automatically analyzed by the Cardea SOLO software and an easy to read and interpret report is generated in five minutes,” he said, “eliminating the need to wait for a third-party report and enabling us to provide a quick diagnosis and expedite treatment if necessary.”
In addition, these next-generation devices are easier to apply, so this process can be managed by non-cardiologists and physicians’ staff members. Application also does not require a high-touch examination and procedure, which is less concerning to patients worried about COVID-19.
Russak had a patient reporting atypical chest pain that didn’t appear to be cardiac in nature, but the man was concerned about going into the office. Russak applied the Cardea SOLO device and drew blood while the patient remained in his car. The test results revealed that the patient was indeed experiencing a cardiac event.
What the Technology is Teaching
Schmidt’s practice covers a sprawling multi-state area that includes all of Oklahoma and parts of Texas and Kansas. “Patient convenience matters,” he said. At-home monitoring allows him to be more effective with telemedicine for AFib patients, whether they are concerned about COVID or live far away from the office. The new Cardea SOLO ECG sensor is easier for patients to wear over several days and provides more data than older-generation devices.
“Lightweight, water-resistant cardiac monitors are not just about convenience, however — they’re changing the way cardiologists manage their patients,” Schmidt said. “The biggest issue I see in maintaining patients’ heart health is that we don’t monitor long enough, especially when it comes to AFib. We can be too passive with intervention, but too aggressive with anticoagulants, which can be dangerous when taken over time.”
He noted that with extended rhythm monitoring, he is comfortable taking patients off medication if they are not experiencing AFib. “We’ve been able to reduce anticoagulant use in our patients by 40 to 50 percent through extended monitoring,” he added. “It really allows us to fine-tune our treatment program.”
In the age of COVID and social distancing, a new generation of wearable ECG monitoring devices is coming into its own at a time when it is most needed. “We acted quickly to provide patients and physicians with essential and easy-to-use telehealth solutions. Whether in-office or via telehealth, Cardea SOLO ECG makes it simpler for both patients and physicians, ultimately reducing the diagnostic and treatment timeline of patients potentially at risk of cardiac arrythmias, like AFib, from weeks to just days,” said Cardiac Insight CEO Brad Harlow.
Reference:
1. According to CDC statistics, about 655,000 Americans die from heart disease each year. Current CDC projections for U.S. COVID-19 deaths in 2020 will number around 240,000 by mid-November, less than half that number.
Related Wearable ECG Monitoring Content:
Moving Beyond Holter ECG: The Rise in Next Generation Technology
How Advances in Wearable Cardiac Monitors Improve the Patient and Clinician Experience
Cardea Solo Wearable ECG Collects High-altitude Cardiac Data on Denali Expedition
Cardiac Insight Partners With VivoSense for Cardiovascular Research
Wearable Cardiac Monitors Are Effective for Tracking Atrial Fibrillation Following Ablation
As Interpretation Criteria Evolve, False Positive Athlete ECG Screening Rates Can Decrease



 March 20, 2024
March 20, 2024