Despite their best efforts, many patients tend to develop heart failure after an acute event (e.g., a heart attack or a viral cardiomyopathy). Upon hospitalization, their condition can advance with possibly irreversible and progressive organ damage. Heart failure (HF) is associated with a high level of disability, healthcare costs and mortality – about 50 percent of patients will die within five years from diagnosis. [1,2] However, a new tool that may help cut costs by avoiding acute care episodes and hospital readmissions is the use of automated tracking of patient-generated health datatracking (PGHD).
Heavy Burden of Heart Failure
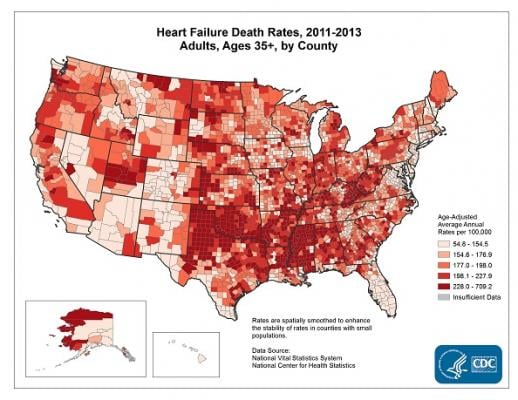
People in their forties have 20 percent risk to develop a heart failure. As stated in the report from the American Heart Association and the Center for Disease Control
(CDC) heart failure fact sheet,[3] about 5.7 million U.S. adults have had HF in 2016.
The number of HF patients, along with the condition complexity, translates into a massive financial burden. It is $38 billion, or 43 percent of annual Medicare spending. The readmission rate also adds to the burden, as more than 25 percent of hospitalized HF patients will be readmitted within 30 days of discharge.
Following the study of medical and socio-environmental predictors of hospital readmission published in the American Heart Journal,[4] some of the potential-readmission signs include:
• Illness severity
• LOS for more than seven days
• Comorbidities, such as hypertension, inflammation, atrial fibrillation and more
Researchers also note that the lack or insufficiency of follow-ups strongly affects the chance of readmission, because regular communication with HF patients improves the chances of strictly following the treatment plan, medication adherence, and physical activity recommendations.
State-of-the-Art in HF Readmission Prevention
Excessive readmissions indicate an inadequate approach to care for discharged HF patients, therefore government and commercial payers have defined a 30-day readmission rate as a quality measure for providers. The idea behind the measure is that caregivers would, above all, harness evidence-based medicine, which should include using standard guidelines and
applying the patient health data analysis methods to extract best practice.
However, the methods proposed by payers target less analytic and more process-tuning initiatives, for example:
• Follow-up phone calls
• Streamlined hospital documentation exchange with PCPs
• Timely access to care after discharge
• Medication reconciliation
• Appropriate medications prescribed
• Patient education at discharge
While these activities are important for readmission rate decrease, they still do not support the effective continuity of care after an HF patient is discharged. While phone calls can give nurses an insight into a patient’s current needs, it is simply not enough.
For example, when the nurse calls, a patient might answer that he or she feels a little weak and tired. That is okay if you are a freshly discharged patient, anything can be a reason for your fatigue, the nurse comforts. But what if an hour later this person develops shortness of breath or starts to feel a headache? These two can be symptoms of hypertension, which may result in hypertensive crisis. In this case, a patient needs immediate medical attention and will be most likely hospitalized.
The point here is if providers were analyzing any changes in the patient’s blood pressure, pulse and temperature, they would be informed and then communicated with this patient in a more effective way, knowing how exactly they could help.
How Patient-Generated Health Data can be a Life Saver for HF Patients
Health data analytics is key to monitoring a patient’s post-discharge recovery and preventing acute events or exacerbations of comorbidities. The good thing is providers already have patient health data in the electronic health record (EHR).
EHR information, including that on comorbidities, vitals, lab results, medical images, distributed medications, procedures and other data, creates the basis for a treatment plan and also helps providers to establish acceptable and target ranges in vitals for a particular patient.
However, EHR is only the starting point. Upon discharge, a patient enters the oblivion zone, where it seems better for them stay, since leaving the zone can mean an appointment or even hospitalization.
To reduce the risk of developing acute events leading to readmission, providers can enable an additional health information source – patient-generated health data (PGHD). PGHD is the subjective and objective data gathered by a patient or their relatives using medical devices or smart wearables and usually reported via mHealth apps.
PGHD Provides Objective Data on Heart Failure
To monitor an HF patient’s health status changes, the following vitals or objective can be measured continuously:
• Weight
• Pulse
• Systolic blood pressure
• Diastolic blood pressure
• Temperature
These vitals can be recorded using smart watches, scales, fitness trackers, pulse meters, blood pressure monitors and other gadgets. An examples of this include specialized wearable HF monitors. The CoVa Monitoring System necklace is worn two minutes a day and measures heart rate, respiration rate, impedance and posture. This data gets to a gateway and then to a Web-based monitoring system. Another example is the SensiVest, which measures absolute lung fluid content, allowing providers to adjust patient medication levels and help individuals to stay on track of their treatment goal.
When aggregated, this data can be then sent to the organization’s health data analytics system to process the results and compare them to previous measurements. If the analysis uncovers negative trends in the patient’s health status, e.g., a sudden or steady gain in daily weight as well as increased heart rate, systolic or diastolic blood pressure, it will automatically notify the care team about possible health risks (via e-mails or text messages).
Of course, a patient or their relatives will be able to get valuable information on vitals too, within the mHealth app. It can be a visualization of changes in each measurement and overall trend backed up with automated push notifications in case of possible health risks.
Subjective Data Analysis in Heart Failure
To facilitate recovery, it is important to keep an eye on subjective information as well. Subjective can be tracked in various ways, for example, in a self-check list with signs and symptoms a patient should identify, journalize and take specific actions if needed. The list of subjective can include:
• Dyspnea
• Coughing or wheezing
• Lack of appetite, nausea
• Edema
• Tiredness, fatigue, decrease in exercise and activity
Aware of the changes, a patient and their family members can gain more control over patient’s health and recovery process. Providers, in their turn, can adjust the treatment plan and help a patient to achieve better health outcomes in a shorter period of time, reducing the risk of readmission.
Case Examples PGHD in HF
Here is how PGHD can help to prevent hospitalization in HF patients.
For example, a patient is weighted daily, and this information goes into the provider’s health data analytics system. The trend shows that the patient gains weight too quickly. The patient’s care team gets an automated notification about this change via an e-mail or text. Since this gain could mean that the body is retaining fluids, the caregiver can conclude that the diuretics prescribed are not efficient enough. Here, the provider can contact a patient or their family to discuss the situation and prescribe another diuretic.
In another case, a patient experiences trouble with breathing, feels lightheaded and dizzy. He or she measures the pressure and the reading signals the prehypertension level (e.g., 139/85). A provider gets this information in the automated notification and also sees the patient’s subjective – dyspnea, fatigue. Not willing to take any risks, a provider also checks the patient’s treatment information from the EHR and contacts the patient or their relatives to advise on a particular medication (e.g., beta-blockers or ACE inhibitors). If the patient’s health status is alarming, a nurse can come to make an injection for a quicker relief.
This way, preventing extremely critical situations, PGHD can help HF patients to recover after discharge and avoid readmissions.
Challenges of PGHD Analysis for Heart Failure Patients
Being a fairly new source of patient health data, PGHD brings in a number of challenges to consider and solve. From the clinical perspective, providers need to take into account the following question points:
• Patient data compilation
• Patient data presentation
• Conducting a meaningful trend analysis
• Enabling interoperability of data across disparate systems and technologies
• Handling internal staff training and primary education for a patient (their relatives) on how to measure and share data
• Adopting an appropriate technology for PGHD processing
• Supporting efficiency in workflows after PGHD adoption
• Elaborating the strategy of dealing with non-standardized devices and software protocols that have not been vetted by the clinical community
Moreover, providers would also need to think through the possible patient-side challenges, should they arise:
• Privacy and security of patient information
• Device reliability, calibration, and accuracy of software to retain and distribute results
• Disclosure or use of PGHD to unintended third parties
One of the essential challenges that needs to be overcome is interrupted measurements and incomplete data. Providers need to take into account that patients are only people, and sometimes they can forget about the need to journalize subjective, sometimes they would feel well and want to skip on measuring blood pressure and pulse this time. In this case, analytics should not output errors and send false reports.
For example, any gaps in weight measurements in the middle of the week can be balanced out with the linear regression for the entire week. In any case, analytics should find the way to extract valuable information and delivering credible output.
Not Perfect, But Another Tool to Help
While using PGHD for HF readmission prevention is not a silver bullet, it is a way to be on the proactive side of care. The post-acute patients are in need of more effective and timely measures to deal with the symptoms, painful experience, negative trends and vitals. Being able to track heart rate, pulse, weight, temperature and subjective, providers can intervene early, so that patients would successfully recover and continue to live their life.
References:



 February 15, 2022
February 15, 2022