Diluting of a blood sample for real-time deformability cytometry testing. Researchers at the Max-Planck-Zentrum für Physik und Medizin in Erlangen. Germany, were able to show for the first time COVID-19 significantly changes the size and stiffness of red and white blood cells, sometimes over months.
July 15, 2021 — Using real-time deformability cytometry, researchers at the Max-Planck-Zentrum für Physik und Medizin in Erlangen were able to show for the first time COVID-19 significantly changes the size and stiffness of red and white blood cells, sometimes over months. These results may help to explain why some affected people continue to complain of symptoms long after an infection, which has become know as long COVID.
Shortness of breath, fatigue and headaches, some patients still struggle with these long-term effects of a severe infection by the SARS-CoV-2 coronavirus after six months or more. This post COVID-19 syndrome, also called COVID long-haulers, is still not properly understood. What is clear is that during the course of the disease, often blood circulation is impaired, clotting and dangerous vascular occlusions can occur, and oxygen transport in is limited. These are all phenomena in which the blood cells and their physical properties play a key role.
To investigate this aspect, a team of scientists led by Markéta Kubánková, Jochen Guck and Martin Kräter from the Max-Planck-Zentrum für Physik und Medizin, the Max Planck Institute for the Science of Light (MPL), the Friedrich Alexander University Erlangen-Nuremberg and the German Centre for Immunotherapy, measured the mechanical states of red and white blood cells.
"We were able to detect clear and long-lasting changes in the cells, both during an acute infection and even afterwards," reports Professor Guck, currently managing director of MPL. The research group has now published their results in the renowned Biophysical Journal.[1]
To analyze the blood cells, they used a self-developed method called real-time deformability cytometry (RT-DC), which has recently been recognized with the prestigious Medical Valley Award. In this method, the researchers send the blood cells through a narrow channel at high speed. In the process, the leukocytes and erythrocytes are stretched. A high-speed camera records each of them through a microscope, and custom software determines which cell types are present, and how big and deformed they are. Up to 1,000 blood cells can be analyzed per second. The advantage of the method is that it is fast and the cells do not have to be labelled in a laborious procedure.
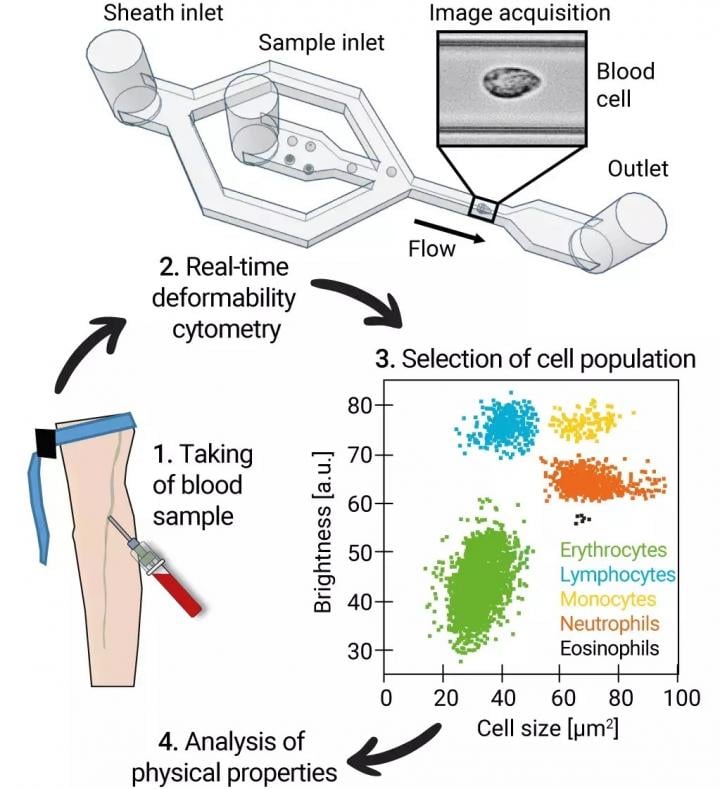
Treatment of blood samples to measure physical properties of leukocytes and erythrocytes. MPL/Guck Division. From the study How a COVID-19 Infection Changes Blood Cells in the Long Run.
The method could help as an early warning system to detect future pandemics by unknown viruses
The biophysicists from Erlangen examined more than 4 million blood cells from 17 patients acutely ill with COVID-19, from 14 people who had recovered and 24 healthy people as a comparison group.
They found that, for example, the size and deformability of the red blood cells of patients with the disease deviated strongly from those of healthy people. This indicates damage to these cells and could explain the increased risk of vascular occlusion and embolisms in the lungs. In addition, the oxygen supply, which is one of the main tasks of the erythrocytes, may be impaired in infected persons.
Lymphocytes (one type of white blood cell responsible for the acquired immune defense) were in turn significantly softer in COVID-19 patients, which typically indicates a strong immune reaction. The researchers made similar observations for neutrophil granulocytes, another group of white blood cells involved in the innate immune response. These blood cells even remained drastically altered seven months after the acute infection.
"We suspect that the cytoskeleton of immune cells, which is largely responsible for cell function, has changed," explains Markéta Kubánková, first author of the research article. In her view, real-time deformability cytometry has the potential to be used routinely in the diagnosis of COVID-19, and even to serve as an early warning system against future pandemics caused by as yet unknown viruses.
Related COVID Long-hauler Content:
VIDEO: What Are The Long-term Cardiac Impacts of COVID-19 Infection — Interview with Todd Hurst, M.D.
The Long-term Cardiovascular Impact of COVID-19
VIDEO: Lingering Myocardial Involvement After COVID-19 Infection — Interview with Aaron Baggish, M.D.
Tsunami of Chronic Health Conditions Expected Due to COVID-19 Disruption of Healthcare
Cedars-Sinai Launches Clinic to Manage Long-Term Heart Health Issues in COVID-19 Patients
VIDEO: Antithrombotic Prophylaxis in COVID-19 Patients — Interview with Behnood Bikdeli M.D.
COVID-19 Registry Tracks Cardiac Health of College Athletes
Coronavirus Disease 2019 (COVID-19) and the Heart—Is Heart Failure the Next Chapter?
Heart Damage Found in More Than Half of COVID-19 Patients Discharged From Hospitals
Overview of Randomized Trials of Antithrombotic Therapy for COVID-19 Patients
COVID-19 Can Kill Heart Cells and Interfere With Contraction
References:


 October 09, 2019
October 09, 2019