October 19, 2011 - A new study published in Circulation: Cardiovascular Interventions shows lesions with large lipid cores are associated with a 50 percent risk of heart attack in patients undergoing coronary stent implantation.
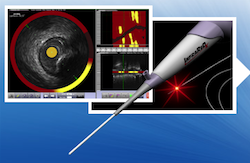
Near-infrared spectroscopy (NIRS) with the InfraReDX LipiScan system was shown to rapidly and accurately detect extensive lipid core plaques (LCPs) that are linked to an increased risk of heart attack during or following percutaneous coronary intervention (PCI). The system is the first and only system approved by the U.S. Food and Drug Administration (FDA) to provide interventional cardiologists with a chemogram, a two-dimensional map of LCP, within the imaged vessel using NIRS.
"Although PCI routinely achieves excellent angiographic results, too many cases continue to suffer from peri-procedural no-reflow and myocardial infarction," said James A. Goldstein, M.D., FACC, director of research and education, division of cardiology, Beaumont Hospital, Royal Oak, Mich., and lead author of the study. "This study utilizing InfraReDx's first-generation LipiScan system with NIR spectroscopy permitted immediate identification of large lipid core plaques known to complicate stenting and suspected to cause most heart attacks. By identifying and quantifying these dangerous plaques that are prone to embolization, the LipiScan system holds the potential to improve patient outcomes and prevent complications in cardiac procedures."
PCI is associated with a peri-procedural heart attack in three to 15 percent of cases. In many cases, these heart attacks result from distal embolization of LCP contents. These heart attacks are detected by procedural elevations of cardiac biomarkers specific for death of heart muscle tissue. LCP is a fatty coronary artery plaque suspected to be vulnerable to rupture, to cause most heart attacks and to complicate stenting procedures either during or post-intervention. Peri-procedural heart attacks are associated with adverse long-term outcomes and in some cases cause immediate adverse events.
The published study shows that in patients with coronary artery disease, PCI of lesions with a large lipid core is associated with a 50 percent risk of heart attack during or post-procedure compared to only a 4.2 percent risk for lesions without a large lipid core. A
large LCP was defined as a maximum lipid core burden index (LCBI) within a 4mm segment of ?500, which corresponds to a LCP which on average is 4 mm long and occupies 180 degrees of the vessel circumference. Sixty-two patients meeting study criteria were selected from the COLOR Registry (NCT00831116). There were no major adverse events attributed to the use of the LipiScan system.
The use of NIR spectroscopy with the LipiScan Coronary Imaging System permitted the immediate identification and quantification of LCPs whose presence could not be determined by coronary angiography. Baseline variables also correlated poorly with the presence of a large LCP, with elevation of plasma LDL levels as the only statistically significant association. Patients with a large LCP had a 12-fold increase in relative risk (95 percent CI 3.3 to 48, p=0.0002) of peri-procedural heart attacks. In contrast, plaque complexity identified on coronary angiography, a finding often considered to be an index of increased risk of a PCI-induced complication, was associated with a relative risk of only 3.5 (CI 0.91 to 14), a difference that was not statistically significant.
Results of the published study are consistent with prior findings with other intracoronary imaging methods, but the LipiScan System identified a much higher relative risk and requires no offline analysis or expert interpretation. These findings support the concept that LCPs may be prone to complications after stenting, and their detection in the catheterization lab prior to angioplasty may help guide the interventional treatment strategy. As stated in the study article, "the ability to identify stenoses with varying levels of risk of complications when stented would indicate that LCP presence or absence might play a role in determining whether or not a lesion should be treated."
The paper titled "Detection of Lipid-core Plaques by Intra-Coronary Near-Infrared Spectroscopy Identifies High Risk of Peri-Procedural
Myocardial Infarction" was published online at http://circinterventions.ahajournals.org/content/early/2011/10/04/CIRCINTERVENTIONS.111.963264.abstract and appears in today's print edition of the journal.
Editor’s note: James A. Goldstein, M.D., is a consultant for and owns equity in InfraReDx Inc.
For more information: www.infraredx.com


 January 05, 2026
January 05, 2026 









