July 18, 2019 — On June 30, 2019, the Centers for Medicare & Medicaid Services (CMS) announced the Johns Hopkins University School of Medicine has been designated a qualified provider-led entity (qPLE). This allows Johns Hopkins to develop criteria that meet the requirements of the federal Protecting Access to Medicare Act (PAMA) of 2014 when ordering diagnostic imaging tests such as computed tomography (CT) scans, magnetic resonance imaging (MRI) scans and nuclear imaging in the emergency department and ambulatory settings.
Johns Hopkins joins 21 other institutions across the nation that CMS has formally approved to design these criteria.
“We are honored by this approval, as it dovetails nicely with our effort to improve the value of medical care in our health system and across the nation,” said Pamela Johnson, M.D., vice chair of quality and safety in the Department of Radiology, professor of radiology and radiological science at the Johns Hopkins University School of Medicine and director of the High Value Practice Academic Alliance. “Our goal is to deliver healthcare of the highest quality, safety, efficiency and effectiveness for our patients. By helping doctors and advanced practice providers use evidence in the literature at the point of care to know which tests to order, which treatments to prescribe and when patients can safely be discharged from the emergency department, we aim to avoid unwarranted variation in care and avoid unnecessary use of medical resources that does not add value, while delivering the best outcomes for our patients.”
Physicians learn best practices during their training. However, as healthcare and technology evolve and improve, medical best practices also must change. And while professional societies publish clinical practice guidelines annually, adopting change can be slow. “Studies estimate that it takes an average of 17 years for new evidence in the literature to translate into changes in practice by the greater medical community,” said Johnson. “We wanted to skip that 17-year delay and improve healthcare quality as quickly as possible so our patients start benefiting right away.”
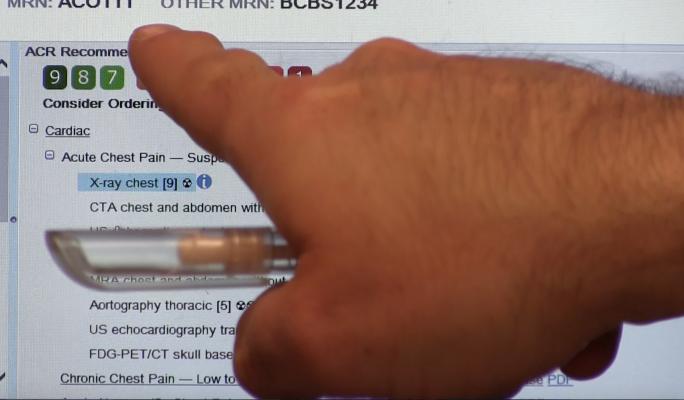
Even before the Johns Hopkins University School of Medicine was designated a qualified provider-led entity, Johnson and colleagues had established teams of physicians from multiple specialties to review primary medical literature and identify the best data to use to design the criteria. After mining the data and writing the criteria, the Johns Hopkins teams integrated them directly into diagnostic decision-making guidelines in the electronic medical record (EMR) system used by the hospitals and ambulatory practices in the Johns Hopkins Health System. From the EMR system, clinicians can access calculators, forms, consultation guides, videos and other resources to make it easier to locate the latest knowledge and best practices when they diagnose and treat patients. To optimize care delivery for each patient, decision trees guide selection of tests and treatments according to clinical symptoms.
This effort resulted in more than 70 guidelines addressing both diagnosis and management for a range of clinical scenarios, such as chest pain and syncope, which have already been built into The Johns Hopkins Hospitals’ emergency department electronic medical record system. Preliminary analyses confirm improvements in care delivery — for example, adhering to the chest pain guideline reduced the number of patients with noncardiac chest pain who were admitted to the hospital unnecessarily. All Johns Hopkins Health System adult emergency departments are now implementing these guidelines.
Johns Hopkins’ new qPLE status will allow its experts to write criteria that can be used to guide physicians’ use of diagnostic imaging tests as required by the CMS Appropriate Use Criteria (AUC) Program, beginning with eight clinical priority areas:
-
Chest pain;
-
Pulmonary embolism;
-
Neck pain;
-
Low back pain;
-
Shoulder pain;
-
Hip pain;
-
Headache; and
-
Lung cancer.
Johns Hopkins plans to make the criteria available to other care providers across the nation by January of next year, when CMS will require all healthcare professionals to consult clinical decision support tools when ordering advanced diagnostic imaging tests for Medicare patients.
“While CMS is focused on advanced diagnostic imaging tests, we at Johns Hopkins are keen to ensure best practice across all aspects of medicine and surgery both within our institution and nationally,” said Johnson. “Our rigorous evidentiary literature review coupled with the clinical expertise of the multidisciplinary teams will hopefully refine the practice of medicine so that patients get tests and treatments that add value to their care and benefit from advances in practice more efficiently than they have traditionally.”
For more information: www.hopkinsmedicine.org
Related Content
New Appropriate Use Criteria Released for Peripheral Artery Interventions
CMS Proposes Delaying Clinical Decision Support Documentation to 2019
Outlining How Artificial Intelligence May Help Adhere to Cardiac Care Guidelines

 February 16, 2026
February 16, 2026