Getty Images
March 13, 2022 – People with a congenital heart defect who were hospitalized with COVID-19 infection were at higher risk for severe illness or death than those without a heart defect, according to new research published in the American Heart Association’s flagship, peer-reviewed journal Circulation. Researchers found people with a congenital heart defect who contracted COVID-19 were also more likely to require treatment in the intensive care unit (ICU) or need a ventilator.
Among those at the highest risk for the most severe COVID-19 illness were patients who had a heart defect and another health condition, were ages 50 and older, or were men, according to the study.
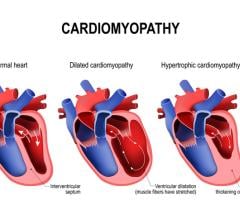
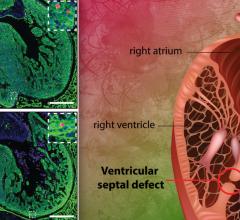
There are more than a dozen types of congenital heart defects, which result when the heart, or blood vessels near the heart don’t develop normally before birth. According to the American Heart Association’s Heart Disease and Stroke Statistics—2022 Update, congenital heart defects are the most common birth defect worldwide, with a global prevalence of 157 per 100,000 in 2017.
“Data comparing COVID-19 outcomes among individuals with and without congenital heart defects has been limited,” said lead author Karrie Downing, M.P.H., an epidemiologist at the National Center on Birth Defects and Developmental Disabilities and the COVID-19 Response Team at the U.S. Centers for Disease Control and Prevention in Atlanta.
Researchers examined data on hospitalized COVID-19 patients from March 2020 to January 2021, collected in the Premier Healthcare Database Special COVID-19 Release, a database representing approximately 20% of all U.S. hospitalizations. The COVID-19 patients with and without heart defects in this study received care in the same hospitals. Differences in age, gender, race/ethnicity, health insurance types and other high-risk conditions (specifically heart failure, pulmonary hypertension, Down syndrome, diabetes and obesity) were accounted for across those populations.
During this period, the database had more than 235,000 patients, ages 1 to 64 years old, who were hospitalized for COVID-19. Patients were divided into two groups: those who had a congenital heart defect and those who did not. Across these two categories, researchers then determined how many required an admission to the ICU, needed a ventilator to help with breathing or died. Researchers also reviewed other characteristics including other health conditions.
Of the 235,638 hospitalized COVID-19 patients evaluated for this study, 421 or 0.2% had a congenital heart defect. The analysis found:
- among the patients with a heart defect, most were over the age of 30 (73%), and 61% were male; 55% were non-Hispanic white people, 19% were Hispanic people and 16% were non-Hispanic Black people;
- overall, 68% of the patients with a heart defect also had at least one other health condition noted, compared to 59% among those without a congenital heart defect;
- 54% of patients with a congenital heart defect were admitted to the ICU compared to 43% of those without a congenital heart defect;
- 24% of patients with a congenital heart defect required a ventilator to breathe compared to 15% of those without a congenital heart defect; and
- 11% of patients with a congenital heart defect died during hospitalization compared to 7% of those without a congenital heart defect.
In addition, people with congenital heart defects consistently remained at high-risk for severe COVID-19 illness, even when divided into categories by age or other health conditions noted in the study, according to the researchers.
Downing believes these findings have immediate, practical relevance for health care professionals as the COVID-19 pandemic continues to evolve: “People with heart defects should be encouraged to receive the COVID-19 vaccines and boosters and to continue to practice additional preventive measures for COVID-19, such as mask-wearing and physical distancing. People with heart defects should also consult with their health care teams about additional steps to manage personal risks related to COVID-19, given the significantly increased risk of severe infection and serious complications.”
Downing noted that not all patients with heart defects who were hospitalized with COVID-19 had poor outcomes. “More work is needed to identify why the clinical course of COVID-19 disease results in significantly worse outcomes for some hospitalized patients with risk factors for critical COVID-19 illness, like heart defects, and not for others,” she said.
There are several limitations to this study. Only people already hospitalized with COVID-19 were included, the clinical details about the underlying heart defect were not available, and lab testing to identify and/or confirm COVID-19 diagnoses may vary by hospital. Lastly, COVID-19 vaccination status was not considered, since the vaccines became available in the U.S. starting in December 2020.
Co-authors are Regina Simeone, Ph.D.; Matthew Oster, M.D., M.P.H.; and Sherry Farr, Ph.D. Authors’ disclosures are listed in the manuscript.
For more information: www.heart.org
Related COVID-19 Cardiology Content:
The Long-term Cardiovascular Impact of COVID-19
COVID-19 Changes Properties Blood Cells
VIDEO: Antithrombotic Prophylaxis in COVID-19 Patients — Interview with Behnood Bikdeli M.D.
Coronavirus Disease 2019 (COVID-19) and the Heart—Is Heart Failure the Next Chapter?
PHOTO GALLERY: How COVID-19 Appears on Medical Imaging
Heart Damage Found in More Than Half of COVID-19 Patients Discharged From Hospitals
Overview of Randomized Trials of Antithrombotic Therapy for COVID-19 Patients
COVID-19 Can Kill Heart Cells and Interfere With Contraction


 March 31, 2025
March 31, 2025