March 27. 2019 — A newly released expert consensus statement provides recommendations for the safe and effective dissemination of newly approved patent foramen ovale (PFO) closure technologies. The document, developed by the Society for Cardiovascular Angiography and Interventions (SCAI) and affirmed by the American Academy of Neurology (AAN), was published online in SCAI’s official journal, Catheterization and Cardiovascular Interventions.
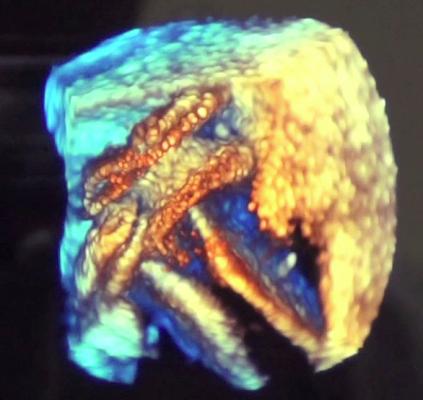
Nearly 25 percent of the general population may have a PFO, which is an opening between the top left and right chambers of the heart. Closure of the PFO is one strategy in mitigating the risk of recurrent stroke in PFO patients who have experienced a cryptogenic stroke. Stroke is the fifth most common cause of death and the leading cause of preventable disability in the United States.
“Completion of the randomized trials demonstrating the superiority of PFO closure and medical therapy over medical therapy alone for appropriately selected patients with cryptogenic stroke and a PFO was a landmark achievement that has resolved decades of uncertainty,” said Eric Horlick, M.D., FSCAI, chair of the paper’s writing group and an interventional cardiologist at the Peter Munk Cardiac Centre, University of Toronto.
The writing group makes specific recommendations in the paper for operator competencies and training, facility infrastructure, multidisciplinary collaboration, and quality assessment measures. “The appropriate use of PFO closure has the potential to change the natural history of a potentially devastating disease process. SCAI and AAN representatives collaborated to help cardiologists and neurologists provide the highest standard of care,” Horlick said.
“SCAI can now confidently offer evidenced-based recommendations for the treatment of these patients, who are seeking answers to guide their therapeutic decision making after a potentially catastrophic event. I am very proud of the work produced by our dedicated and highly experienced SCAI writing group, including representatives from the AAN. The resulting document is pragmatic and aims to inform and assist clinicians and institutions in maintaining an evidenced-based, patient-centered approach to the care of this patient population with a focus on quality and safety.,” he continued.
The U.S. Food and Drug Administration (FDA) recently approved two percutaneous PFO occluder devices. Prior to approval, closure devices had only been available off-label through a humanitarian device exemption, and in randomized clinical trials. Now approved, the devices are widely available.
Related PFO Closure Content:
VIDEO: How Transcatheter PFO Closure Can Reduce Cryptogenic Stroke — Interview with John Rhodes, M.D.
VIDEO: An Overview of PFO Closure to Treat Cryptogenic Stroke — Interview with Karen Orjuela, M.D.
VIDEO: Transcatheter Closure of Holes in the Heart — Interview with Ziyad Hijazi, M.D.
VIDEO: Demonstration of a Transcatheter PFO Occluder Implantation
VIDEO: Addressing Adult Congenital Heart Referrals — Interview with Ami Bhatt, M.D.
Reference:


 November 14, 2025
November 14, 2025 









