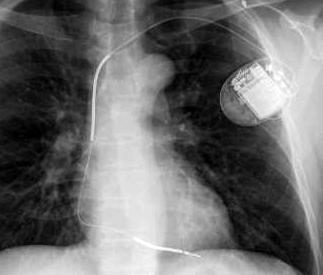
January 18, 2010 – A 10-year follow-up of patients with implantable cardioverter defibrillators (ICDs) will determine long-term outcomes of ICD therapy in heart failure patients.
The SCD-HeFT 10-Year Follow-up Study will revisit 1,855 patients who participated in the original SCD-HeFT (Sudden Cardiac Death in Heart Failure Trial) to determine long-term outcomes 10 years after their last recorded follow-up. The study will be led by Gust H. Bardy, M.D., at the Seattle Institute for Cardiac Research (SICR), who was also the principal investigator in the original SCD-HeFT.
The original study proved the effectiveness of ICD therapy over placebo or amiodarone to treat irregular heartbeats. The results were instrumental in changing the national reimbursement policy for ICD therapy. SCD-HeFT outcomes remain a key reference point for all other ICD evaluations for patients with congestive heart failure (HF). The trial was conducted from 1997-2003 and studied 2,521 patients with HF for an average follow-up period of 45.5 months. It was and remains the largest, longest and only placebo-controlled, randomized, multicenter trial ICD therapy.
At the time of the presentation of the SCD-HeFT findings in March 2004, the patients who had not yet received an ICD were given the option to receive one. It is estimated, however, that few of the patients in the placebo or amiodarone groups ultimately received an ICD, essentially maintaining the original study groups of HF patients treated either with ICD or non-ICD therapies. As a result, long-term results of these two patient groups can likely still provide significant findings regarding the long-term efficacy of ICD therapy.
Today marks the median 10-year anniversary of follow-up for the SCD-HeFT population. The follow-up study will attempt to investigate all surviving patients and those who have succumbed since the end of the original trial by recontacting the 148 institutions participating in the trial (136 in the U.S., 11 in Canada and one in New Zealand). The follow-up data obtained in this project will be merged with the original SCD-HeFT database collected during the original trial, thus providing a long-term follow-up profile on all patients that were enrolled.
“The outcome of SCD-HeFT changed medical practice, but despite the virtues of the trial, many key questions remain regarding long-term efficacy, complications and cost of ICD therapy,” said Dr. Bardy. “We believe the results of this study have the potential to help direct long-term ICD management for the foreseeable future.”
The primary goals of the follow-up study are to compare 10-year mortality data for the three arms of the trial (ICD, placebo and amiodarone); use rates and complication rates; lead failure rates and replacement rates; and to gather 10-year hospitalization, major procedure data, and quality of life data. The study will also obtain outcome data in the major subgroups: ischemic versus non-ischemic; New York Heart Association (NYHA) Class II HF versus NYHA Class III HF; and in women and minorities.
The study is being sponsored by the National Heart, Lung, and Blood Institute, part of the National Institutes of Health, and St. Jude Medical Inc.
For more information: www.sjm.com


 January 05, 2026
January 05, 2026 









