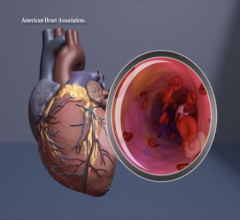
COVID-19 has a big impact on the heart, and patients with pre-existing cardiovascular disease have at least a 10 percent higher risk of death and severe complications due to the virus. The virus also can cause myocarditis, blood clotting, and impact the cardiovascular system due to severe, hyperactive inflammatory responses. Left, a cardiac CT scan 3-D rendering. right, the COVID-19 virus from a National Institutes of Health (NIH) photo.
August 17, 2020 - The number of people coronavirus disease 2019 (COVID-19) is rising with more cases in the U.S. There are more than 5 million SARS-CoV-2 cases in the United States according to the Centers for Disease Control and Prevention (CDC), more than any other country, and more than 20 million confirmed cases worldwide, according to the World Health Organization (WHO).
Initially thought to be an infection causing disease of the lungs, inflammation of the vascular system and injury to the heart appear to be common features of this novel coronavirus, occurring in 20 to 30 percent of hospitalized patients and contributing to 40 percent of deaths.[1] The risk of death from COVID-19-related heart damage appears to be as or more important than other well-described risk factors for COVID-related mortality, such as age, diabetes mellitus, chronic pulmonary disease or prior history of cardiovascular disease.[2,4]
“Much remains to be learned about COVID-19 infection and the heart. Although we think of the lungs being the primary target, there are frequent biomarker elevations noted in infected patients that are usually associated with acute heart injury. Moreover, several devastating complications of COVID-19 are cardiac in nature and may result in lingering cardiac dysfunction beyond the course of the viral illness itself,” said Mitchell S. V. Elkind, M.D., MS, FAHA, FAAN, president of the American Heart Association (AHA), the world’s leading voluntary organization focused on heart and brain health and research, and attending neurologist at NewYork-Presbyterian/Columbia University Irving Medical Center. “The need for additional research remains critical. We simply don’t have enough information to provide the definitive answers people want and need.”
COVID Compared With Other Viruses
Compared with other major viral outbreaks in recent memory, including severe acute respiratory syndrome (SARS-CoV-1) in 2002-2003, the pandemic of COVID-19, which is caused by a novel coronavirus termed severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), appears to be less fatal, but it spreads more easily.[2] Adults over age 60 are likely more susceptible to contracting the infection and more likely to die when they do. However, researchers do not yet know why older people are more likely to get sick.[3]
COVID-19 Causes Exaggerated Inflammatory Response
While the majority of COVID-19 patients appear to recover well, a smaller number experience severe, exaggerated inflammation throughout the body, known as a cytokine storm. This systematic inflammation, which is carried through and affects the entire vascular system, is seen in the most severe cases and at the advanced stage of the illness. It can lead to widespread blood clotting, organ failure and/or damage to the heart or other organs. Similarly generalized inflammation likely contributes to a condition known as Multisystem Inflammatory Syndrome in Children (MIS-C), seen in a small number of children with COVID-19 who displayed Kawasaki disease-like symptoms. Symptoms of this syndrome are fever, abdominal pain, gastrointestinal complaints and rash. Myocarditis and meningitis can occur, and patients may have circulatory collapse and respiratory failure.
Read the related article Kawasaki-like Inflammatory Disease Affects Children With COVID-19
Angiotensin-converting Enzyme Involvement in COVID-19
COVID-19 enters cells by binding to the angiotensin-converting enzyme 2, or ACE2, a component in the body’s vascular system that controls blood pressure and may contribute to the development of cardiovascular issues.[1] The relationship between viral entry and ACE2 had led to controversy surrounding the use of drugs which interfere with the renin-angiotensin-aldosterone system, thereby increasing the level of ACE2 and theoretically increasing susceptibility to infection. However, credible animal models of viral infection have shown that higher ACE2 levels may be protective by providing a backlog of receptors to offset those lost during the infection.[4,5]] And human studies have not shown greater susceptibility to or severity of infection among those taking drugs that affects ACE2.
In March, the AAHA, the Heart Failure Society of America (HFSA) and the American College of Cardiology (ACC) jointly recommended continuation of angiotensin converting enzyme inhibitors (ACE-i) or angiotensin receptor blocker (ARB) medications for all patients already prescribed those medications for indications such as heart failure, hypertension or ischemic heart disease. The statement — which remains valid today — indicates that patients with cardiovascular disease who are diagnosed with COVID-19 should be fully evaluated before adding or removing any treatments, and any changes to their treatment should be based on the latest scientific evidence and shared-decision making with their physician and health care team.
Read the related article ESC Council on Hypertension Says ACE-I and ARBs Do Not Increase COVID-19 Mortality
Quarter of Hospitalized COVID Patients Experience Serious Cardiovascular Complications
Nearly a quarter (23%) of people hospitalized for COVID-19 have experienced serious cardiovascular complications. Studies have shown 8% to 12% of all COVID-19 patients have acute cardiac injury. There are also case studies that indicate COVID-19 may lead to heart attacks, acute coronary syndromes, stroke, blood pressure abnormalities, clotting issues, diffuse myocarditis (heart muscle inflammation) and fatal arrhythmias (irregular heartbeats). Based on studies of similar viruses, researchers speculate that heart complications are possible even after recovery from COVID-19.[6] Two recent small German studies found heart muscle abnormalities months after patients had recovered.[7] While the incidence of these complications is not fully known, and it remains unclear how much cardiac injury is due to direct COVID-19 infection of the heart muscle or a result of immune mediated cardiac dysfunction following a profound viral illness, the virus does have a critical influence on the cardiovascular system.[8] There is concern that SARS-CoV-2 may have lasting or even delayed effects on the cardiovascular and nervous systems, a possibility that requires further investigation.
Cardiovascular Impact of Drugs Used to Treat COVID-19
Previously, the American Heart Association warned of the potential harm to the heart from use of the antiviral and antimalarial agent hydroxychloroquine as a COVID-19 treatment. At that time, the association indicated further evaluation is necessary to justify routine use of hydroxychloroquine as a treatment — that remains the case today. More research is needed before hydroxychloroquine can be recommended for COVID-19. People should not take any forms of hydroxychloroquine or chloroquine, or azithromycin, without a full evaluation by their doctor and a careful assessment of the potential harms. The U.S. Food and Drug Administration (FDA) has recommended against further study of these treatments given concerns about harms from the medications.
Read the related article FDA Reports of Deaths and Injuries From Use of Antimalarial hydroxychloroquine in COVID-19 Patients
Additional Research Needed to Better Understand Cardiovascular Impact of Coronavirus
Clearly, additional scientific research on COVID-19 and the heart and vascular system is needed. The AHA has worked to help fill that need. As part of its global response to the growing COVID-19 pandemic, the AHA committed $2.5 million to research efforts to better understand this unique coronavirus and its interaction with the body’s cardiovascular and cerebrovascular systems. Earlier this month, additional grants were awarded to help unlock the mysteries of the impact on the heart. In addition, the association stood up the Get With The Guidelines COVID-19 CVD Registry to capture data on patient clinical characteristics, medications, treatments, laboratory data, biomarkers and outcomes in adult patients hospitalized with COVID-19, including those without a history of cardiovascular disease or stroke. Currently more than 150 U.S. hospitals are participating contributing nearly 14,000 patient records, and the list of contributing hospitals is growing.
The American Heart Association said it will continue to seek new ways to address the cardiovascular complications of the virus through research and education of the public and professionals. The AHA said its registry and other ongoing efforts, including additional research funding, will uncover novel ways to understand and treat this pandemic and its heart implications and future diseases.
Related Cardiac COVID-19 Content:
The Cardiovascular Impact of COVID-19
Autopsies Reveal Surprising Cardiac Changes in COVID-19 Patients
How Cardiology Dealt With the COVID-19 Surge in New York City
Kawasaki-like Inflammatory Disease Affects Children With COVID-19
New Research Highlights Blood Clot Dangers of COVID-19
Additional COVID-19 Resources on Cardiology From the AHA:
- American Heart Association coronavirus (COVID-19) resources
- American Heart Association COVID-19 newsroom
- American Heart Association coronavirus (COVID019) resources for health care professionals
- Immunotherapy, steroids had positive outcomes in children with COVID-related multi-system inflammatory syndrome
- Circulation “On My Mind” post on MIS-C in adults https://www.ahajournals.org/doi/pdf/10.1161/CIRCULATIONAHA.120.050166
References:
1. Shi S, Qin M, Shen B, For, 2020]. JAMA Cardiol. 2020. doi: 10.1001/jamacardio.2020.1017.
8. Strokes: JAMA Neurol 4/10/2020) Arrhythmia and myocarditis: JAMA Cardiology, 03/27/20 and Shi S, JAMA Cardiol 3/25/20


 November 14, 2025
November 14, 2025