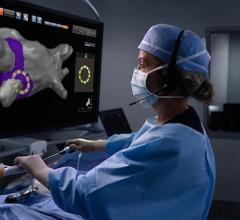
Boston Scientific's Apama multi-electrode ablation balloon to treat atrial fibrillation. The technology allows different energies to be used for each electrode to prevent damage to the esophagus or other underlying critical structures.
The development of atrial fibrillation (AFib or AF) ablation technologies over the past 20 years has been a constant exercise to build a better mouse trap. The goal has been to improve patient outcomes, reducing the need for repeat procedures and to reduce procedure times. However, despite these advances and two decades of experience, long-term procedural success rates at curing persistent AF are about 50-60 percent at 18 months.[1] Ablation to treat paroxysmal AF has better outcomes, but it still may require repeat procedures to finish the job. In addition, these procedures can be very time-consuming to perform electromapping and the ablation procedure itself, sometimes taking hours.
New atrial fibrillation ablation technologies recently commercialized or in trials may offer new hope for increasing long-term procedural success and in reducing procedural times.
“It is a very exciting time in the field of AF ablation,” said Hugh Calkins, M.D., FACC, FAHA, FHRS, director of cardiac arrhythmia services and professor of medicine at Johns Hopkins Hospital, past Heart Rhythm Society (HRS) president and lead author of the HRS AF consensus document. “If you look at what has happened since it was developed about 20 years ago, it keeps getting better, the outcomes continue to get better, the safety keeps getting better. The adoption of the procedure is now widespread and internationally it is growing at an extremely high rate.”
However, he explained AF ablation still has a ways to go and there is a need for new technologies.
“It is still not a perfect procedure,” Calkins said. “Part of that is because we do not have a perfect understanding of the mechanisms of atrial fibrillation, and part of that is because we do not have perfect tools. We know that our current results are not where we need to be. I hope in five years the single-procedure efficacy in an optimal patient is at 80 percent with a shorter, more reliable procedure. If we could accomplish that, it would be a huge step forward. Right now it is more like 60 percent.”
The main goal in AF ablation is centered on electrical isolation of the pulmonary veins. Calkins said the workhorse systems for this today are the cryoballoon, radiofrequency (RF) ablation and contact force sensing catheters.
Use of Contact Force-sensing Ablation Catheters to Improve Lesion Effectiveness
Studies found the contact force of an ablation catheter against tissue is a big factor in whether the lesion created will be effective in blocking conduction. This has lead to the rapid adoption of force-sensing catheters that can show the amount of pressure being applied during ablations, which has led to improved outcomes and fewer repeat procedures.[2-4]
“We have had contact force sensing catheters for several years now, but it has gotten better and better,” said Michael Gold, M.D., Ph.D., director of cardiology and associate dean at the Medical University of South Carolina (MUSC) and immediate past president of HRS. “We can gauge the contact we are making to avoid ineffective lesions because we are not making sufficient contact, and to minimize complications because we are not having excess contact against the wall of the heart.”
Calkins said the Biosense Webster SmartTouch and the Abbott TactiCath contact force sensing catheters have become the standard in RF ablation technology. “They are good, but they are still not perfect,” he explained.
The main issue with point ablation catheters is that EPs must play a game of connect-the-dots by creating dozens of single-point ablations, overlap these lesions, and do this without the ability to directly see what they are doing and while the heart is in constant motion. This leaves a lot of room for sub-optimal ablations, which often account for 40 percent or more of patients needing repeat procedures to re-isolate the pulmonary veins.
“I think one of the biggest frustrations with AF ablation is if you take patients who have failed one procedure back to the EP lab and most studies will tell you that 70-80 percent of these patients will have at least one vein that has reconnected,” Calkins explained.
Balloon Ablation Catheter Technologies Help to Speed Procedure Time and Lesion Effectiveness
Balloon ablation catheters have been developed to help eliminate the need for connecting multiple ablation points and to help shorten procedures. This has led to the development of the Medtronic Arctic Front Cryoballoon family of balloon-based, one-shot cryro-ablation catheters. The balloon can perform faster and more effective vein isolations with a single balloon inflation and application of refrigerant to freeze the tissue. Clinical data shows the technology reduces repeat procedures by 33 percent, with reduced complications compared to RF.[5]
Calkins said the rapid adoption of the cyroballoon is partly due to its ability to shorten procedure times and ablate in a more predictable, reproducible fashion.
The latest clinical data on cryoballoon ablation presented at HRS 2017 was an economic analysis from the landmark FIRE and ICE trial. The data show that treating paroxysmal AF with the cryoballoon may result in substantial cost savings as compared to RF ablation. These findings were driven by fewer repeat ablations and cardiovascular rehospitalizations in patients treated with the cryoballoon and were consistently observed in multiple healthcare systems internationally included in the analysis.[6]
The most commonly reported adverse event with cryoballoons is phrenic nerve injury, which occurred in 2.7 percent of patients in the FIRE and ICE trial, the most recent study for the device.[2] The nerve damage is due to the close proximity of the nerve to the pulmonary vein and the equal distribution of cooling around the pulmonary vein. This has led to some next-generation ablation systems in development to take this into account and allow for different energies to be delivered to areas where there are underlying critical structures.
“There is lots of new technology coming to allow us to electrically isolate the pulmonary veins in a more constant way,” he said.
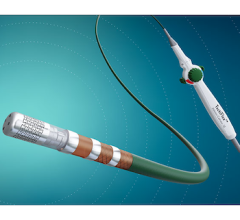
One of the most promising technologies is RF ablation balloons that use a series of flexible electrodes to isolate the pulmonary vein in one inflation. These are being developed by both Biosense Webster and Boston Scientific (Apama Medical RF balloon catheter system).
The RADIANCE study, presented at HRS 2017, was a 39-patient first-in-human study for the Biosense Webster RF balloon technology. It showed the device could uniformly achieve PVI in all patients without the need for "touch-up" with a focal ablation catheter. The study showed the RF balloon catheter could deliver directionally-tailored energy using multiple electrodes for efficient acute PVI in patients with paroxysmal AF.[7]
Another promising technology is the CardioFocus HeartLight laser balloon catheter, Calkins explained. The system uses direct visualization through a video camera in the catheter to direct a laser to perform the ablation.
HeartLight was granted U.S. Food and Drug Administration (FDA) clearance in 2016. The system’s compliant balloon seats in the ostia of the pulmonary veins and a laser inside the catheter can be rotated around to ablate the tissue. Its direct visualization of the procedure eliminates the need for electro-mapping systems and cuts procedural time. The lesions are created with 20-30 second ablations. About 25 ablations are needed to isolate a pulmonary vein with lesion overlap. The combination of the balloon, camera and variable-energy, steerable ablation is believed to be able to eliminate the interoperator variability in ablation procedures. Another advantage of the system is that it can deliver variable energy, so the energy of the laser can be dialed down when ablating near the esophagus or other neighboring critical structures.
UPDATE May 2020 — FDA Clears HeartLight X3 Laser Ablation System to Treat Atrial Fibrillation
Research Into New Targets for AF Ablation
“The big, huge challenge we have is the ablation of persistent, long-standing AFib, where the results are clearly inferior to the ablation results for paroxysmal atrial fibrillation,” Calkins said.
There was a period where there was a lot of emphasis placed on CFAEs [complex fractionated atrial electrograms] being performed to treat persistent and longstanding persistent Afib and linear ablations in addition to PVIs, but data from the STAR AF II study showed there was no benefit to these techniques and PVI alone was sufficient, Calkins said. “That has launched what I would call the modern period of AF ablation, which is coming up with new ablation strategies to target new substrates,” he explained.[8]
One of the biggest areas for these new strategies is mapping and targeting the dynamic substrate of AF rotors. Calkins said Topara led this effort with some initial studies that were very positive, but later had some studies that were not as positive. He said Topara (now owned by Abbott) is currently conducting several randomized, controlled trials to finally determine what is the true incremental efficacy of doing rotor mapping and ablations.
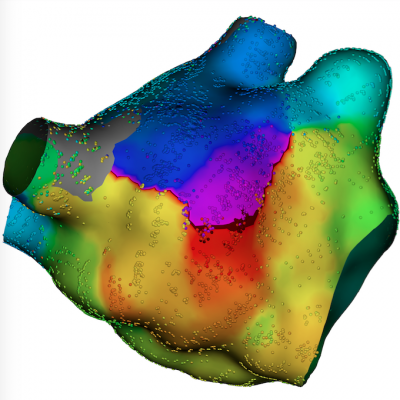
Another new technology is surface body mapping, which combines a 252-lead electrocardiogram (ECG) vest with a computed tomography (CT) scan to create detailed combined 3-D cardiac anatomy with overlaid electromapping. Calkins said this technology can also identify rotor activity noninvasively and be used for pre-procedure planning. Medtronic received FDA clearance for the CardioInsight Noninvasive 3D Mapping System in early 2017.
Watch a VIDEO of how the CardioInsight electro-anatomical mapping system works
There also are some early studies looking at ablating areas of scar to eliminate possible re-entry circuits.
“There are early studies coming out saying that voltage-based identification of scar and ablating these areas might matter… but until we have prospective randomized, multicenter clinical trial data, you have to take these small, positive studies with a grain of salt. This does not mean one technology is better over another. Ultimately we need to perfect these systems and then subject them to the proper clinical trials to look at their true clinical value."
Improved EP Electromapping Systems
Part of the issue with accuracy and need for repeat procedures may be due to in part to how EPs visualize the anatomy, electrical activity and the placement of lesions using electromapping systems. The standard has been using point-by-point mapping where EPs push a catheter against the wall of the atrium to PV to record electrical activity. Hundreds of these point recordings are needed to create an electro map of the anatomy. However, the new generation of systems use basket catheters to rapidly record thousands of points, which make the electro maps much more accurate.
“Mapping systems are just exploding in terms of more accurate mapping, being able to map more quickly to see where circuits are, look for rotors, and look for other potential mechanisms causing arrhythmias that make us more effective and efficient,” Gold said.
The first vendor to introduce a high-density mapping system was Boston Scientific with its Rhythmia system in 2014. The vendor released the updated Rhythmia HDx at HRS 2017. It can show lower voltages than on previous-generation mapping systems and uses a 64-electrode basket catheter to create very detailed, high-density electro-maps with as many as 50,000 to 60,000 points. “The Rhythmia system was the first high-density mapping system to come out and really put pressure on the other companies to come out with their own high-density mapping systems,” Calkins said.
At HRS 2017, St. Jude/Abbott introduced the new Ensite Precision high-density mapping system that is designed to reduce shift and drift to improve AF ablation. The system gained FDA clearance in December 2016 and includes the launch of the Advisor mapping catheter, which incorporates magnetic sensing technology. This works with a magnetic sensor placed under the patient to more accurately locate mapping points and the tip of the catheter inside the anatomy. It also helps increase the accuracy of the anatomical model of the heart the system creates to guide procedures. St. Jude said this has eliminated distortion of the model that was a drawback of the previous-generation system.
A new technology that may offer a big reduction in mapping/procedural times is the Acutus Medical AcQMap High Resolution Imaging and Mapping System. It uses a basket catheter with 48 electrodes combined with 48 tiny ultrasound transducers. The basket can be manually rotated around inside the atrium to rapidly “paint” a very accurate combined electro- and anatomical map simultaneously in about five minutes. Conventional EP mapping systems can take 20 minutes or longer to complete the mapping process. The electrodes do not need to contact the walls of the heart because the vendor said they can detect the electrical field created by cardiac contractions. The system was cleared by the FDA in October 2017 and has had European market clearance since 2016.
Watch a VIDEO demonstration of the AcQMap high-resolution EP mapping system
Biosense Webster also exhibited its new work-in-progress high-density system at HRS 2017.
“All of the mapping systems are getting better,” Calkins explained. “The whole field is moving toward more accurate mapping, more points and clearer electrograms. Hopefully this will translate into better efficacy for our patients. As someone who spends a lot of time doing catheter ablations, I welcome all these new mapping technologies. We want shorter procedures and better, safer procedures, and all of this will help us get there.”
Future Electrophysiology Ablation Technologies on the Horizon
Calkins said there are three technologies being researched that may offer new treatment avenues in AF. The first is the use of magnetic resonance imaging (MRI) in place of angiography and electromapping systems to directly visualize catheters and the tissue reaction to ablations, including being able to see the depth of the lesions made. Several centers around the world are using prototype MRI-guided EP ablation labs, including one at the National Institutes of Health (NIH).
“The promise is enormous, the promise of doing these procedures with no radiation, being able to see the lesions, being able to see the anatomy is unbelievably attractive,” Calkins said.
The other technology area being researched is use of automated, fully-robotic, externally applied radiation therapy or focused ultrasound to ablate the heart without the need to catheterize the patient. These systems use patient MRI or CT scans to create a treatment plan and place energy beams where they avoid critical structures. The treatment plan is then used by the system’s computer to guide the therapy after the patient is precisely registered in the table with the imaging of the treatment plan.
Calkins said the company CyberHeart Inc. is working on this system. The company is currently recruiting for a 10-patient study to test the system for noninvasive cardiac ablation for refractory ventricular tachycardia/fibrillation. The two centers with the investigational technology are MedStar Health Research Institute in Washington, D.C., and the Texas Cardiac Arrhythmia Research Foundation based in Austin.[9]
A similar approach is to use focused ultrasound, usually guided by MRI, which follows a similar treatment planning process as radiation therapy. Focused ultrasound directs ultrasound energy beam pulses from different directions that converge in the tissue to be ablated. Focused ultrasound is already FDA-cleared to ablate some types of cancer.
Another technology being investigated is electroporation, where tailored electrical charges are used to open pores in the cell walls of the targeted tissue to cause cell death. Calkins said the process keeps the tissue intact without charring or exploding the cells from rapid heating. Different tissues have different susceptibility to electroporation, so it can be used to target specific issues, while not causing damage to other tissues around the target area.
Related Content on AF Ablation Technologies
Expert Consensus Released on Catheter, Surgical Ablation of Atrial Fibrillation
VIDEO: Current State of Atrial Fibrillation Ablation Technologies, an interview with Hugh Calkins, M.D., at HRS 2017.
VIDEO: Editor's Choice of Most Innovative New Technology at HRS 2017
What is New in Electrophysiology Technologies
New Data and Technology To Treat Atrial Fibrillation
Meeting the Treatment Demands of a Growing AFib Epidemic
Patient Information on What is AFib and Treatment Options
Treatment Options of Atrial Fibrillation (AFib or AF) — American Heart Association
Managing Atrial Fibrillation with Medication
The Basics to Understanding the Dioagnosis and Treatment of Atrial Fibrillation (NIH website)
How to Treat Afib, Treatment Options (Cleveland Clinic)
References:



 January 22, 2026
January 22, 2026