Increased radiation exposure seems inherent to TR access, but may be outweighed by the numerous advantages of this approach.
Recently, concerns have been raised that transradial (TR) cardiac catheterization significantly increases radiation exposure when compared with the conventional transfemoral (TF) approach. The current rapid uptake of TR in the United States is mainly due to its economic benefits and overall favorable patient outcomes. Perhaps most importantly, TR provides a measurable reduction in vascular complications, which translates to shorter time for ambulation and post-procedural stay. The reduction in bleeding with TR likely lowers mortality in patients with ST-elevation myocardial infarction (STEMI). One potential reason for the slow adoption of TR may be the perceived concern about increased radiation exposure.
Before reviewing the available data it is important to stress that with any approach, it is prudent to adhere to the ALARA (as low as reasonably achievable) principle. This can be accomplished by maintaining exposure at as low a level of radiation as possible by increasing the distance from the source of radiation, decreasing exposure duration and using all available shielding.
Variability in Studies
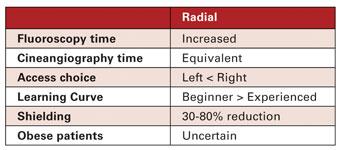
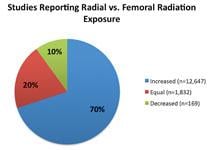
The current literature is not consistent about the exposure with TR and TF approaches. The majority of published studies (70%) reported an increase in radiation exposure to both operator and patient with TR compared with TF access. Others have reported findings suggesting no significant difference (20%), and a minority (10%) reported decreased exposure with TR access. (Figure 1.) While these studies may not be directly comparable, it appears that TR is associated with overall increased radiation exposure to the operator and patient when compared to the TF approach.
Fluoroscopy exposure during TR appears increased and several observational and randomized studies suggest differences in radiation exposure to patients between TR and TF catheterization. These differences in fluoroscopy times between TR and TF access underscore the increased time that is needed to navigate the tortuous subclavian vessels and to engage the ascending aorta. Cine-angiography times and exposures, on the other hand, are comparable between TF and TR approaches. While cine-angiography delivers a higher dose of radiation, its contribution to total radiation dose during percutaneous coronary intervention (PCI) may be variable, as more time is spent performing fluoroscopy.
Quantifying Radiation Exposure
While the operators are exposed repeatedly to ionizing radiation, the one-time increase in exposure to the patient remains low. Placed into perspective, the difference in diagnostic studies between TR and TF access has been estimated at just 0.4 mSv — corresponding to 20 chest X-rays. The alternative view is that this increase in radiation exposure with TR translates into an increase in lifetime cancer risk to the patient of just 0.002%.[1]
The impact of patient body weight on radiation exposure during TR is quite interesting. Operators may choose to perform TR on morbidly obese patients and thus introduce significant bias toward observed greater exposure with TR. At this time, the available data in the literature remains somewhat inconclusive, as some studies found positive correlation between body mass index (BMI) and TR ionizing radiation exposure, and some did not.
Interestingly, while patient exposure has been reasonably well researched, the evidence on operator exposure is limited. Published studies report a pastiche with either lower, equal or higher operator exposure with TR. Nonetheless, in the largest and most representative study that studied 16 highly experienced high-volume operators in a tertiary referral center, it appears that radiation exposure was higher for TR. The most fascinating finding was that “low-exposure” TR operators were also “low-exposure” TF operators.[2] Practice patterns and practice styles appear thus to play a very important, yet difficult-to-quantify role in radiation exposure with either access.
Right or Left Radial?
The question frequently arises whether to chose a left or right TR approach. With the left approach it is generally easier to engage the coronary ostia. Studies suggest either lower[3] or equal radiation with the left TR approach. There are no studies suggesting higher exposure with the left TR approach. This is consistent with the generally simpler navigation through the shoulder and less tortuous left subclavian vessels.
As expected, radiation shielding works well for TR approach. Radiation doses can be reduced from 30% up to 80% with dedicated drapes and shielding boards.[4] Somewhat surprisingly, increasing distance from the radiation source by adding extension tubing did not result in lower exposures to the operator. Power injectors will likely afford quite welcome ability to distance oneself from the source of radiation.
Practice makes perfect and that is true in the radial arena as well. The data in the literature nicely supports that more experienced operators are consistently able to achieve lower radiation exposure.[5]
Benefits Outweigh Risks
Ultimately, with current techniques, increased radiation exposure seems inherent to TR access. Nonetheless, when considering the numerous advantages of TR access, radiation exposure remains just one of many factors when deciding whether to go radial or femoral. Further research should help us better understand how to balance the radiation risks with the vascular access complication reductions afforded by TR access. It is quite likely that new imaging equipment, new dedicated radial catheter designs and new shielding solutions will reduce radiation dose currently observed with TR approach.
Editor’s note: Mladen I. Vidovich, M.D., FACC, FSCAI, is associate professor of medicine, University of Illinois at Chicago, and chief of cardiology at the Jesse Brown VA Medical Center in Chicago. He can be reached at [email protected].
Read the article “Radial Access, Same-Day Cardiac Procedure Could Save $300 Million Annually.”
Watch the video “Update on U.S. Transradial Access Adoption With Sunil Rao at TCT 2015,” a discussion with Sunil Rao, M.D., associate professor of medicine and a member in the Duke University Clinical Research Institute, and a leading proponent of radial access.
Read the article "Software to Help Manage Medical Imaging Radiation Dose."
References:
5. Looi JL, Cave A, El-Jack S. “Learning curve in transradial coronary angiography.” Am J Cardiol. 2011;108:1092-1095.


 October 24, 2025
October 24, 2025