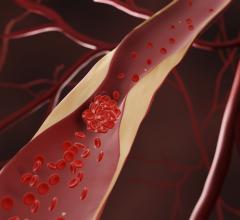
February 22, 2017 — If hospitals can perform more transradial, same-day percutaneous coronary intervention (PCI), hospitals across the U.S. could collectively save $300 million each year, according to research published recently in JACC: Cardiovascular Interventions. The procedure is also better for patients as it results in fewer health complications.
Currently, balloon angioplasty and stenting are some of the leading national expenditures for cardiovascular procedures. PCI costs the U.S. approximately $10 billion each year. There has been little data on strategies that can be implemented to help reduce costs of PCI.
“We now have identified a mechanism for hospitals to improve their efficiency and lower costs, and which is associated with improved PCI outcomes simultaneously,” said the study’s lead author Amit P. Amin, M.D., MSc, assistant professor of medicine at Washington University School of Medicine in St. Louis. “Our data show there is a tremendous potential to reduce costs of PCI, reduce complications and achieve a ‘win-win’ for both patients and hospitals. Hospitals that redesign their care pathways to perform more same-day, transradial PCIs can potentially save hundreds of thousands of dollars each year.”
The study evaluated different PCI approaches and care pathways to see which would be least costly. Researchers examined nearly 280,000 Medicare patients in the National Cardiovascular Data Registry’s (NCDR) CathPCI Registry undergoing PCI who were eligible for same-day discharge. Out of this group, the arm artery access was used in 9 percent of the patients, and same-day discharge was used in 5.3 percent of patients. The adjusted cost associated with arm access with same-day discharge was $13,389 while the cost associated with leg access with overnight stay was $17,076, a difference of $3,689 per PCI procedure.
The study goes on to point out that by shifting practice by 30 percent for more same-day arm access procedures, a hospital performing 1,000 elective PCI procedures per year could reduce costs by approximately $1 million. If collectively all hospitals across the country followed this care pathway, PCI costs would be lowered by almost $300 million annually.
“One hope is that professional medical organizations will take these findings into account when developing new PCI treatment guidelines, and consider the benefits for both the patient and the health care system as a whole,” Amin said. “Also, we need to continue to pursue research like this — in all areas of medicine — that demonstrates ways in which higher quality care can be delivered at a lower cost, to elevate the value of health care that our patients deserve.”
While selection bias can never be completely ruled out with registry-based outcomes research, every possible attempt to reduce this bias through appropriate exclusions and statistical methodology was made to ensure that the study population was eligible for same day discharge, according to the authors.
Read the article “Radial Access Adoption in the United States.”
Watch the VIDEO “Update on U.S. Transradial Access Adoption With Sunil Rao at TCT 2015”
Related NCDR CathPCI Registry articles:
• New Report Highlights National Trends in Heart Disease Treatments
• Better Prognosis for Some PCI Patients When Operators Perform More Procedures
• Study Finds Significant Variability in Doctors' Angioplasty Death Rates
Reference
Amin, A.P., Patterson, M., House, J.A., Giersiefen, H., et al. "Costs Associated With Access Site and Same-Day Discharge Among Medicare Beneficiaries Undergoing Percutaneous Coronary Intervention: An Evaluation of the Current Percutaneous Coronary Intervention Care Pathways in the United States," JACC: Cardiovascular Interventions. Published online ahead of print Feb. 20, 2017. DOI: 10.1016/j.jcin.2016.11.049


 July 31, 2024
July 31, 2024