U.S. positive COVID test case data for 2020 through June 3, 2021, It shows four clear waves of spikes in U.S. COVID cases. Most of these appeared to be partly fueled by people gathering during the July 4, Halloween, Thanksgiving, Christmas, New Year's, Valentine's Day, and easter holidays. Source: Johns Hopkins University
Vaccinations appear to to be helping reduce COVID-19 virus positive case numbers, and a review of the U.S. COVID positive testing data data shows holiday gatherings played a key role in the virus spread.
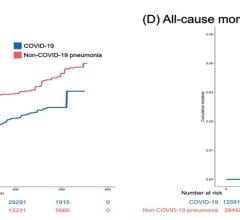
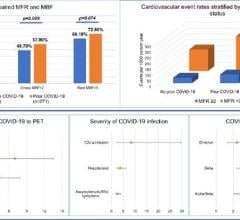
Looking at the U.S. COVID-19 positive test data from the Johns Hopkins University of Medicine website that is tracking world-wide COVID data, there were four district waves of COVID infection in the chart. The initial infections in March-May 2020, a larger spike after the July 4 holiday, and then a steady rise starting around Sept. 10 through mid-February 2021. Numbers then started to slowly drop until March 22, then they rose again through April 15 and then dropped off to what we have today, with the lowest numbers of positive cases reported since March 2020 at the start of the pandemic.
It is very possible the fourth wave, between March and April, was blunted by the most vulnerable populations being vaccinated by then and most states opening up general population vaccinations as of early to mid-April.
The largest spike in U.S. cases was in the third wave, which started last September and quickly rose from 25,000 cases per day to more than 180,000 cases per day being reported as of Nov. 25. In that rise in cases last fall, the number of cases increased by more than 10,000 a day a few days after Halloween and continue to rise more steeply into November.
During the week of Thanksgiving, it appeared numbers had stabilized and started to drop, but it appeared now this was due to people not getting tested or busy with the holiday and extra days off work. The slight dip in positive cases quickly vanished the first week of December with a sudden spike upward to a high of 222,000 positive cases per day as of Dec. 17. This spike was likely due to many traveling or visiting family during Thanksgiving.
After Dec. 17, the numbers began to drop again to 185,000 new cases reported as of Christmas Day. The numbers of positive tests stabilized and plateaued the week of Christmas, bust started rising again as of Dec. 31. New Years parties and visiting family the week of Christmas likely caused the biggest spike in U.S. cases just after New Years Eve, to a high of 259,000 cases reported on Jan. 9, 2021. The numbers then began to steadily declining for the next month and a half.
In late February, numbers rose a little and slowed the decline that started in January. The rise in cases are likely attributable to the back-to-back lesser holidays of Valentine's Day and Presidents Day. Presidents Day Monday is a day kids are off school in most places and parents often do something as a family over the long 3-day weekend.
Numbers began a slow rise again in March and rose fastest in the week after Easter, which was on April 4, another point when families generally get together or attended church in large numbers. Numbers of positive cases rose to the highest in the fourth wave to 77,000 on April 13. The numbers then started the stead decline to the low numbers until now, with 19,400 new cases reported nationwide as of June 3, 2021. This is the lowest rate since March 2020.
It is clear from the numbers that larger spikes in COVID cases occurred after July 4, Halloween, Thanksgiving, Christmas, New Year's Eve and Easter.
Cases actually continued a slow decline in the week after the three-day weekend of Labor Day. The Memorial Day weekend in late May also did not see a significant increase in cases, which were pretty stable until late June when they began a noticeable, slow rise.
For more COVID data: https://coronavirus.jhu.edu/map.html
COVID Content Related to Cardiology and Medical Imaging:
The Long-term Cardiovascular Impact of COVID-19
VIDEO: ECMO Hemodynamic Support Effective in Sickest COVID-19 Patients — Interview with Ryan Barbaro, M.D.
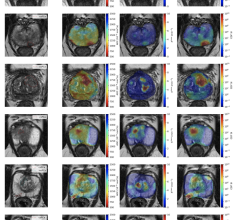
IMAGE GALLERY: How COVID-19 Appears on Medical Imaging
ECMO Support Found Effective in Sickest of COVID-19 Patients
Kawasaki-like Inflammatory Disease Affects Children With COVID-19
VIDEO: Overview of Multisystem Inflammatory Syndrome in Children (MIS-C) in COVID-19 Exposed Children — Interview with Deepika Thacker, M.D.
VIDEO: How to Image COVID-19 and Radiological Presentations of the Virus
Addressing Atrial Fibrillation in the World of COVID-19
VIDEO: What Does COVID-19 Look Like in Lung CT Scans
Overview of Trials for Anticoagulation Therapy for COVID-19 Patients
The Cardiovascular Impact of COVID-19
VIDEO: COVID-19 Pneumonia Chest CT Scan Scroll Through
COVID-19 Blood Vessel Damage May Cause Brain Fog and Other Long-hauler Symptoms
Overview of Randomized Trials of Antithrombotic Therapy for COVID-19 Patients
CDC Updates Its Mask Recommendations
CDC Update on Excess Deaths Associated with the COVID-19 Pandemic

 March 20, 2024
March 20, 2024