September 26, 2019 — New data from the Phase IV independent TWILIGHT trial showed Brilinta (ticagrelor) monotherapy reduced the risk of BARC type 2, 3 or 5 bleeding in high-bleed-risk patients who underwent percutaneous coronary intervention (PCI) and completed three months of dual antiplatelet therapy (DAPT) at 12 months. Brilinta monotherapy (90 mg twice daily) was compared to Brilinta plus low-dose aspirin.
Results from TWILIGHT were presented at 2019 Transcatheter Cardiovascular Therapeutics (TCT annual scientific conference of the Cardiovascular Research Foundation and published simultaneously in the New England Journal of Medicine.[1]
In the trial, 9,006 patients received open-label ticagrelor (90 mg twice daily) and aspirin (81-100 mg daily) for three months after a PCI. The 7,119 patients that remained event-free of major bleeding or an ischemic event during the three months of treatment with ticagrelor and aspirin were randomized to either double-blinded aspirin or placebo for an additional 12 months, with continuation of open-label ticagrelor.
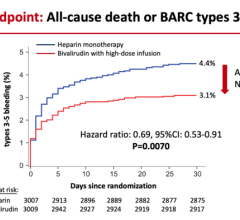
Ticagrelor monotherapy was associated with a 44 percent lower risk of BARC (Bleeding Academic Research Consortium) 2, 3 or 5 bleeding over one year, with an absolute risk reduction of 3.1 percent, compared to ticagrelor plus aspirin. The incidence of the primary endpoint — time to first occurrence of BARC type 2, 3 or 5 bleeding between month 3 and 15 — was 4 percent in patients treated with ticagrelor plus placebo compared to 7.1 percent in patients treated with ticagrelor plus aspirin (HR 0.56; 95 percent CI 0.45 to 0.68; p<0.001).
The incidence of BARC 3 or 5 bleeding was also lower (1 percent vs 2 percent, HR 0.49; 95 percent CI 0.33 to 0.74) with ticagrelor plus placebo versus ticagrelor plus aspirin. Rates of the composite of all-cause death, myocardial infarction (MI) or stroke, a key secondary endpoint, were similar between the two groups — 3.9 percent and 3.9 percent, respectively for ticagrelor plus placebo and ticagrelor plus aspirin (HR 0.99; 95 percent CI 0.78 to 1.25; non-inferiority p<0.001).
Roxana Mehran, M.D., TWILIGHT's global principal investigator and director of the Center for Interventional Cardiovascular Research and Clinical Trials at Mount Sinai Heart and professor of cardiology, and population health science and policy, at Icahn School of Medicine at Mount Sinai, said “In high-risk PCI patients, further ischemic events remain a life-threatening concern. As seen in TWILIGHT, in patients who tolerated three months of dual antiplatelet therapy, lowering the risk of major bleeding while preserving the ischemic benefit using ticagrelor monotherapy is an important clinical advance for these patients.”
VIDEO: TWILIGHT Trial Shows Benefit to Ticagrelor Monotherapy After Stent Implantation — Interview with Roxana Mehran, M.D., at TCT 2019
Watch the VIDEO: Strategies to Avoid Acute Kidney Injury Caused by Cath Lab Contrast, an interview with Mehran
Find information on other late-breaking TCT trials
For more information: www.nejm.org
Reference
1. Mehran R., Baber U., Sharma S.K., et al. Ticagrelor with or without Aspirin in High-Risk Patients after PCI. New England Journal of Medicine, published online Sept. 26, 2019. DOI: 10.1056/NEJMoa1908419

 August 28, 2023
August 28, 2023