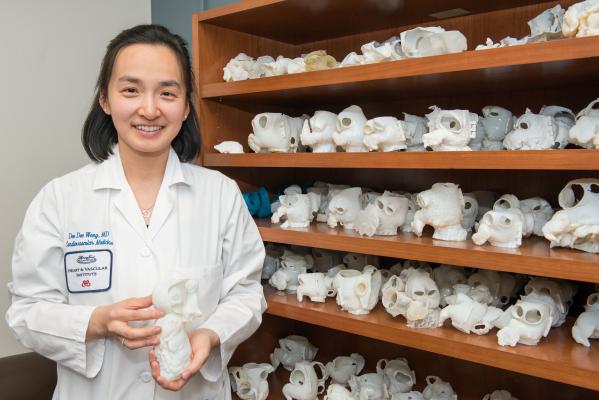
Dee Dee Wang, M.D., runs Henry Ford Hospital's 3-D printing lab that supports its complex structural heart program.
Three-dimensional (3-D) printed anatomic models created from a patient’s computed tomography (CT), magnetic resonance imaging (MRI) or 3-D ultrasound imaging datasets are seeing increasing use for procedural planning and hands-on clinical education. Some cardiovascular centers have created their own 3-D printing labs to enable on-demand printing of complex anatomy not only for planning and device sizing, but also to practice dry runs and aid procedural navigation. An emerging trend is the use of new 3-D computer modeling software to enable virtual device implantations for improved patient selection, to reduce complications, and enable faster development of novel transcatheter devices and procedural techniques.
Building a Cardiac 3-D Printing Program
For centers thinking of creating a 3-D printing program, cardiologists need to ask what they plan to use the models for to determine what they need in terms of printer quality and types of media to make the models, said Vijay Iyer, M.D., Ph.D., director of the complex valve clinic and structural heart interventions at the Gates Vascular Institute (GVI) and Buffalo General Medical Center (BGMC). Iyer helped create a 3-D printing lab at Gates. If the printed models are for educational purposes, these can be printed out of a single color and material. But, if the model will be used for pre-procedural planning, he said a higher-end printer will be needed that can print multiple materials to simulate the actual anatomy. This includes flexible materials for soft tissues and hard plastics to simulate things like calcified valves.
“The ability to do multi-material printing is very important if you are using the models for procedural planning and dry runs,” Iyer said. “We print the entire structure, including the valves, aortic arch and the femoral access points to see the impact of the angulations and vessel tortuosity. If you only print the heart, you don’t have all the anatomy that plays a role in the delivery of the device.”
To start a 3-D printing program, Iyer said a hospital needs physicians who will champion the project and invest time. There also needs to be buy-in from the other physicians so the lab will be used. “It’s not just a shiny new toy, they have to understand its applications and actually use it,” he stressed. He said the biggest value in 3-D printing is being able to see complex anatomy in a new way to better prepare physicians for procedures and to better understand potential complications.
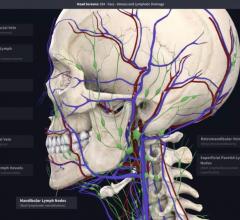
“For someone to really understand the anatomy — even for an experienced cardiologist — they do not always appreciate the complexities by looking at 2-D images from ultrasound, CT scans or angiography,” Iyer explained. “In congenital heart cases, 3-D printing is invaluable. We find it most beneficial in the areas of pre-surgical planning, transcatheter structural heart procedural planning, and education and training.” This includes use for planning, device sizing, and procedural guidance for novel devices and techniques, such as mitral or pulmonic transcatheter valve-in-valve procedures.
“We try to anticipate problems with dry runs using the 3-D printed anatomy,” Iyer said. “We want to answer questions like is a 23 mm valve better than a 26 mm valve, or what are the delivery issues we will likely run into. We sometimes change the sizes of devices or the choice of wires we will use based on the 3-D printed anatomy.”
Gates Vascular Institute often prints 3-D models of patients’ left atrial appendage (LAA) prior to Watchman transcatheter occlusions. Iyer said the shape of the LAA varies tremendously between patients, so careful patient selection is important to prevent embolization. The models help determine the best deployment landing zones and help evaluate the actual 3-D shape, depth and ostium of the LAA, which all play a role in the success of LAA occluder implantations.
Iyer said physicians at the institute have been creative to think of new applications for 3-D printing. One use that was not thought of originally is to print the vasculature of the brain in complex neuro-interventional procedures. This way operators can see if devices fit the anatomy and if they can be successfully navigated through very tortuous anatomy. Physicians also have discussed using 3-D printed coronary vessels with known fractional flow reserve (FFR) readings to bench-test use of various device therapies to see the impact on hemodynamics.
Moving From Static Models to Dynamic Computer Simulations
Henry Ford Hospital in Detroit, Mich., was a pioneer in the use of a 3-D printing lab as part of its renowned structural heart program. “We get a lot of high-risk patients who are turned down by other institutions and because of our heart team and the transcatheter procedures we offer,” said Dee Dee Wang, M.D., FACC, FASE, FSCCT, director of structural heart imaging, medical director 3-D printing, Henry Ford Innovations Institute. Many patients referred to her center are too frail, old or sick to be surgical candidates and they come to Henry Ford as a last resort. For this reason, precision is important, so 3-D printing was adopted to review complex anatomies and new types of procedures.
“There is added value of 3-D printing during procedures, but what we quickly learned was that the real value of 3-D printed anatomy is in the physical shape,” Wang explained. However, she said it was not as impactful in adult structural heart disease or interventions as originally planned.
She said the problem with 3-D models is that it freezes the motion of the heart in a static position. Since the physiology of the heart is constantly moving, a 3-D print cannot predict the exact impact of a procedure on the anatomy or function of the moving heart.
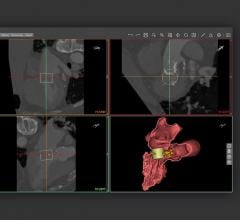
CT imaging can determine what device size to put into a patient, Wang said. “What we were missing is computer-aided design (CAD), because then you have the technology to see depth, angulation, diameters and anatomical constrains,” she explained. For this reason, Henry Ford has been an early adopter of the Mimics Innovation Suite CAD software from the 3-D printing vendor Materialise. This medical-grade software creates dynamic, virtual 3-D models where virtual devices can be placed to look at their impact on hemodynamics, or how the movement of the heart is impacted.
Mitral valve regurgitation (MR) is the No. 1 valvular heart disease. As the U.S. population ages, the patient population for MR and surgical valve procedures is expected to rise rapidly. “However, it is the most high-risk procedure that can cause death on the table,” Wang said. “This is where transcatheter interventions are moving to, and 3-D modeling has two critical roles, which are sizing and identifying LVOT (left ventricle outflow tract) obstruction. This helps us see what we fear. If we undersize a valve it embolizes. If we oversize a valve, it causes LVOT obstruction. We also can have annular disruption, which can tear apart the heart.
“The value in 3-D for us is actually in the computed-aided design,” Wang continued. “We learned we can size the valves using the CAD software. We can overlay a valve and see how it fits. We can take the patient’s CT scan and use computer modeling to try implanting the valves in various positions to find out what valve size we are going to use, and find out what the impact will be on LVOT. We calculate a baseline LVOT surface area to see what level of blood flow they live with, and then we model a valve inside and see what remainder of the LVOT they have left, and we can set a cutoff perimeter. We have done enough of these patients where we now have a curve. Our data is pretty good and we know where the cutoff curve for procedures should be, so we know when to send a patient to hospice and not try to put a valve in them.”
This ability to do computer modeling also is impacting the development of new devices and techniques.
“The real-world impact with CAD-specific modeling, we can now find alternative ways to innovate new technologies,” Wang said. This included the development of a technique using alcohol spatial ablations to make the LVOT bigger, so patients who would have died a year ago during this procedure can now survive. She also said they know if they angle the valves in some patients, this could produce better outcomes for some. This modeling helps tailor the implant procedure to the specific patient. “In the mitral valve, we can kill patients, but patient-specific modeling can help prevent that,” Wang said.
Creating 3-D Printable Files
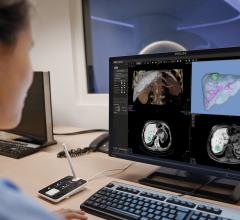
Creating files for 3-D printing from medical imaging datasets starts with good imaging, said Shuai Leng, Ph.D., associate professor of medical physics, Mayo Clinic, Rochester, Minn. “If you start with garbage in, you get garbage out, so you need good image quality.” To create a usable 3-D file, he suggests using 0.6 mm thin imaging slices. This allows for very smooth surfaces. By comparison, he said use of 6 mm slices will make the printed object very rough and textured, appearing pixelated, when it is printed in 3-D.
He said dual-energy CT is great for 3-D printing because it can easily exclude bone so only blood vessels or soft tissue remain in the image area. Metal implants commonly cause problems when creating 3-D printing files, but dual-energy systems have metal artifact reduction software to separate the metal and artifacts from the anatomy to allow creation of better models.
When using 3-D models for procedural planning and navigation, he suggests ensuring the precision of the model by using U.S. Food and Drug Administration (FDA)-cleared 3-D printing software. The resulting printed models also should be compared to the original images to ensure the sizing is correct. Before printing, images should be checked in three planes and approved by a radiologist or the ordering physician.
The final imaging files are converted into STL/CAD files that can be read by the 3-D printers and translated into the final 3-D object.
Partnerships Make 3-D More Accessible
The setup and maintenance costs for 3-D printing can be expensive, especially at centers where there is very limited application. This has led to the creation of partnerships between advanced imaging vendors and 3-D printer vendors to create contract services for one-off printing projects.
Advanced visualization software company Vital Images was the first to develop a partnership with 3-D printer company Stratasys in 2015. Customers can print-on-demand using Vital’s Vitrea advanced visualization software and Stratasys’ 3-D printing services. Vital Images' software takes patient scans and converts them into STL files that can be sent directly to a 3-D printer, improving workflow efficiency and 3-D printing accessibility.
In 2016, TeraRecon partnered with 3-D printing provider WhiteClouds. The workflow process to print highly detailed, full-color 3-D models directly from the TeraRecon software eliminates the step of needing to create an STL file. The goal of the service is to provide a user-friendly workflow with zero startup costs where customers can quickly create high resolution and life-like anatomical models.
Most picture archiving and communication system (PACS) vendors offer STL file conversion to enable 3-D printing from clinical image datasets. Some are taking that ability further with formal partnerships with 3-D printing vendors. A few imaging IT companies, including GE Healthcare and Carestream, have recently partnered with the 3-D printing and software company Materialise to develop a software package that will allow the easy creation of 3-D printable files. Philips Healthcare is in the process of inking a deal with two 3-D printing vendors that it plans to unveil in the fourth quarter of 2017.
Related Cardiovascular 3-D Printing Content:
The Future of 3-D Printing in Medicine
VIDEO: Applications in Cardiology for 3-D Printing and Computer Aided Design
Materialise Announces Start of Pre-Market Phase for Mitral Valve Planning
FDA Changes Rules For Custom Medical Device Exemptions
3-D Printed Heart Technology Aids Diagnosis, Procedural Planning
VIDEO interview with Dee Dee Wang, M.D., explaining the use of 3-D printing to aid procedural planning and guidance in complex structural heart cases.

 May 12, 2020
May 12, 2020