Clive Svendsen, Ph.D., director of the Cedars-Sinai Board of Governors Regenerative Medicine Institute, at work in his laboratory. Photo by Cedars-Sinai.
June 30, 2020 — A new study shows that SARS-CoV-2, the virus that causes COVID-19 (coronavirus), can infect heart cells in a lab dish, indicating it may be possible for heart cells in COVID-19 patients to be directly infected by the virus. The discovery, published today in the journal Cell Reports Medicine, was made using heart muscle cells that were produced by stem cell technology.
Although many COVID-19 patients experience heart problems, the reasons are not entirely clear. Pre-existing cardiac conditions or inflammation and oxygen deprivation that result from the infection have all been implicated. But until now, there has been only limited evidence that the SARS-CoV-2 virus directly infects the individual muscle cells of the heart.
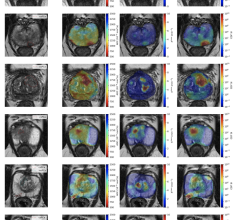
“We not only uncovered that these stem cell-derived heart cells are susceptible to infection by novel coronavirus, but that the virus can also quickly divide within the heart muscle cells,” said Arun Sharma, Ph.D., a research fellow at the Cedars-Sinai Board of Governors Regenerative Medicine Institute and first and co-corresponding author of the study. “Even more significant, the infected heart cells showed changes in their ability to beat after 72 hours of infection.”
The study also demonstrated that human stem cell-derived heart cells infected by SARS-CoV-2 change their gene expression profile, further confirming that the cells can be actively infected by the virus and activate innate cellular "defense mechanisms" in an effort to help clear out the virus.
While these findings are not a perfect replicate of what is happening in the human body, this knowledge may help investigators use stem cell-derived heart cells as a screening platform to identify new antiviral compounds that could alleviate viral infection of the heart, according to senior and co-corresponding author Clive Svendsen, Ph.D.
“This viral pandemic is predominately defined by respiratory symptoms, but there are also cardiac complications, including arrhythmias, heart failure and viral myocarditis,” said Svendsen, director of the Regenerative Medicine Institute and professor of Biomedical Sciences and Medicine. “While this could be the result of massive inflammation in response to the virus, our data suggest that the heart could also be directly affected by the virus in COVID-19.”
Researchers also found that treatment with an ACE2 antibody was able to blunt viral replication on stem cell-derived heart cells, suggesting that the ACE2 receptor could be used by SARS-CoV-2 to enter human heart muscle cells.
“By blocking the ACE2 protein with an antibody, the virus is not as easily able to bind to the ACE2 protein, and thus cannot easily enter the cell,” said Sharma. “This not only helps us understand the mechanisms of how this virus functions, but also suggests therapeutic approaches that could be used as a potential treatment for SARS-CoV-2 infection.”
The study used human induced pluripotent stem cells (iPSCs), a type of stem cell that is created in the lab from a person's blood or skin cells. IPSCs can make any cell type found in the body, each one carrying the DNA of the individual. Tissue-specific cells created in this way are used for research and for creating and testing potential disease treatments.
“This work illustrates the power of being able to study human tissue in a dish,” said Eduardo Marbán, MD, Ph.D., executive director of the Smidt Heart Institute, who collaborated with Sharma and Svendsen on the study. “It is plausible that direct infection of cardiac muscle cells may contribute to COVID-related heart disease.”
The investigators also collaborated with co-corresponding author Vaithilingaraja Arumugaswami, DVM, Ph.D., an associate professor of molecular and medical pharmacology at the David Geffen School of Medicine at UCLA and member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research. Arumugaswami provided the novel coronavirus that was added to the heart cells, and UCLA researcher Gustavo Garcia Jr. contributed essential heart cell infection experiments.
“This key experimental system could be useful to understand the differences in disease processes of related coronaviral pathogens, SARS and MERS,” Arumugaswami said.
These studies were performed under the following approvals: UCLA provided The Human Pluripotent Stem Cell Research Oversight (hPSCRO) #2020-004-01 for Human iPSC-derived cardiac and lung cells for disease modeling COVID-19, as well as protocol BUA-2020-015-003-A approved by the UCLA Institutional Biosafety Committee (IBC).
Funding: Research from the Svendsen laboratory has been supported by the National Institutes of Health under award number 5UG3NS105703 and the Cedars-Sinai Board of Governors Regenerative Medicine Institute. Arun Sharma is supported by an institutional training grant from the NIH under award number T32 HL116273.
For more information: www.cedars-sinai.org
Related Cardiology COVID-19 Content:
United We Stand Against COVID-19 was Overarching Message From ACC 2020 Virtual Meeting
The Cardiovascular Impact of COVID-19
VIDEO: 9 Cardiologists Share COVID-19 Takeaways From Across the U.S.
VIDEO: Why QT-prolongation Occurs in COVID-19 Patients on Hydroxychloroquine and Azithromycin — Interview with Andrew D. Krahn, M.D.,
COVID-19 Hydroxychloroquine Treatment Brings Prolonged QT Arrhythmia Issues
VIDEO: CT and POCUS Emerge As Frontline Cardiac Imaging Modalities in COVID-19 Era — Interview with Geoffrey Rose, M.D.
FDA Revokes Emergency Use Authorization for Chloroquine and Hydroxychloroquine for COVID-19
Cardiology Meetings Continue to be Cancelled or Go Virtual Due to COVID-19
How Cardiology Dealt With the COVID-19 Surge in New York City
Kawasaki-like Inflammatory Disease Affects Children With COVID-19
New Research Highlights Blood Clot Dangers of COVID-19
VIDEO: Impact of COVID-19 on the Interventional Cardiology Program at Henry Ford Hospital — Interview with William O'Neill, M.D.
ACC COVID-19 Clinical Guidance For the Cardiovascular Care Team

 March 20, 2024
March 20, 2024