Getty Images
July 6, 2022 — In one of the first studies to investigate the overall quality of care and outcomes of stroke care for non-COVID-19 hospitalized patients during the pandemic from a national U.S. perspective, researchers from the U.S. Department of Veterans Affairs (VA), Regenstrief Institute and Monash University assessed patients with strokes and transient ischemic attacks (often called mini-strokes or TIAs) in 128 hospitals across the U.S. in the VA’s health system, the nation’s largest integrated healthcare system. The researchers report no decline in overall quality of care nor outcomes (after risk adjustment) when comparing patients with stroke and mini-strokes from prior to the pandemic [March to September 2019] to the same months during the pandemic [March to September 2020].
As with other non-COVID-19 conditions, the number of hospitalizations for strokes and mini-strokes was lower during the pandemic than before COVID-19; approximately 30 percent lower for mini-strokes and 19 percent lower for strokes.
The researchers used seven standardized measures to determine that overall quality of care for stroke and mini-stroke did not diminish in VA facilities during the pandemic. They found that, importantly, the use of statin medications continued to increase during 2020 – especially among patients with stroke – a trend that had been evident for several years prior to the pandemic. However, patients with stroke or mini-stroke had far fewer primary care visits, delaying or deferring care during the pandemic.
During the pandemic approximately 40 percent of stroke patients did not have a blood pressure measurement while only 10 percent of stroke patients pre-pandemic did not have a blood pressure measurement. Missing blood pressure checks was associated with a six-fold increase in short-term mortality and a three-fold increase in long-term mortality, according to VA and Regenstrief Research Scientist Dawn Bravata, M.D., an Indiana University School of Medicine faculty member, who led the study. She notes that a robust relationship between increasing blood pressure and stroke risk has long been known to exist. The researchers found that blood pressure, when measured during the pandemic, was not as well controlled as during the pre-pandemic period.
The study also found that death rates of stroke or mini-stroke patients in VA hospitals were not statistically different after risk adjustment during the pre-pandemic and pandemic time periods.
“As a healthcare system that is responsible for and tracks patients after they are discharged from the hospital, the VA is well suited to conduct this type of analysis and do the follow-up indicated – for example, helping patients control blood pressure after a stroke or ministroke,” said Dr. Bravata. “Given the widespread phenomena that people received less healthcare during the pandemic, we would expect the same decrease in primary care visits in non-VA settings. As patients return to primary care, post-stroke checkups and blood pressure control hopefully can be prioritized.”
With few exceptions, stroke and mini-stroke patient characteristics were similar between 2019 (pre-pandemic) and 2020. The researchers found that during the pandemic, a slightly greater proportion of patients came to the hospital as a result of a stroke, rather than due to a mini-stroke (69 percent versus 66 percent). Dr. Bravata says that individuals with transient symptoms of mini-strokes may have hesitated to seek medical attention during the pandemic.
The study evaluated care for patients with stroke or mini-stroke from typical causes and did not include patients who were admitted to the hospital for COVID-19 and then had a stroke or mini-stroke. Fewer than 2 percent (72 individuals) of those admitted to the 128 VA hospitals with stroke or mini-stroke from March to September 2020 concurrently had or subsequently developed COVID-19.
“Quality of Care and Outcomes for Patients with Acute Ischemic Stroke and Transient Ischemic Attack During the COVID-19 Pandemic” is published in Journal of Stroke and Cerebrovascular Diseases. Authors, in addition to Dr. Bravata, are Laura J. Myers, PhD, and Anthony J. Perkins, M.S., of the VA and Indiana University School of Medicine (U.S.) and Monique F. Kilkenny, PhD, of Monash University and The Florey Institute of Neuroscience and Mental Health (Australia).
This work was supported by the VA Health Services Research & Development Service (HSRD), Expanding Expertise Through E-health Network Development (EXTEND) Quality Enhancement Research Initiative (QUERI) (QUE HX0003205-01).
For more information: https://www.regenstrief.org/
Related Cardiology Content:
In-Hospital Deaths in STEMI Patients With COVID-19 Drop in 2021
The Long-term Cardiovascular Impact of COVID-19
COVID-19 Changes Properties Blood Cells
VIDEO: Antithrombotic Prophylaxis in COVID-19 Patients — Interview with Behnood Bikdeli M.D.
Coronavirus Disease 2019 (COVID-19) and the Heart—Is Heart Failure the Next Chapter?
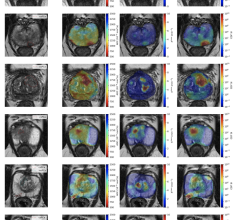
PHOTO GALLERY: How COVID-19 Appears on Medical Imaging
Heart Damage Found in More Than Half of COVID-19 Patients Discharged From Hospitals
Overview of Randomized Trials of Antithrombotic Therapy for COVID-19 Patients
COVID-19 Can Kill Heart Cells and Interfere With Contraction

 March 20, 2024
March 20, 2024