Dapagliflozin did not significantly reduce organ failure or death in high-risk hospitalized COVID-19 patients in the DARE-19 trial results, presented at ACC.21.
May 18, 2021 — Dapagliflozin (Farxiga), a sodium-glucose co-transporter 2 (SGLT2) inhibitor, did not significantly reduce the risk of organ failure or death or improve recovery in patients hospitalized with COVID-19 (SARS-CoV-2) who are at high risk of developing serious complications compared to placebo, according to data presented at the American College of Cardiology (ACC) 2021 Scientific Session.
The researchers, while acknowledging the results were not statistically significant, said they were encouraged by the lower numbers of organ failure and deaths observed in patients treated with dapagliflozin and by favorable safety data.
Dapagliflozin is commonly prescribed in cardiology for heart failure to reduce the risk of needing to be hospitalized and death due to heart and blood vessel disease. The SGLT2 inhibitor was initially developed as a medication to lower blood sugar levels in patients with Type 2 diabetes, but clinical studies have since demonstrated that it also has significant cardiovascular and kidney benefits, regardless of diabetes status.
COVID-19 can lead to multi-organ failure, especially in patients at high risk for severe illness and complications. The Dapagliflozin in Respiratory Failure in Patients with COVID-19 (DARE-19) trial was the first phase III randomized, controlled clinical trial that was initiated to determine whether dapagliflozin could reduce cardiovascular, kidney and respiratory complications or all-cause death and improve recovery (dual primary endpoints), in patients acutely ill and hospitalized with COVID-19.
“We already know that SGLT2 inhibitors provide organ protection in patients with Type 2 diabetes, heart failure and chronic kidney disease, and these are the exact same patients who if they contract COVID-19 are at high risk to be hospitalized with serious illness and develop complications, such as organ failure,” said Mikhail Kosiborod, M.D., cardiologist at Saint Luke's Mid America Heart Institute, vice president for Research at Saint Luke’s Health System in Kansas City, Mo., and the study’s principal investigator. “Accordingly, we wanted to see if dapagliflozin may also help with organ protection in patients with cardiometabolic risk factors who are acutely ill and require hospitalization due to COVID-19.”
“There were concerns at the beginning of the pandemic about the safety of SGLT2 inhibitors in patients hospitalized with COVID-19, and some groups were recommending discontinuation of these medications in this setting, even in individuals with chronic conditions in which they have known benefits, such as Type 2 diabetes and heart failure. Everyone was doing their best to make recommendations for what they felt was the safest approach in a data-free zone at that time,” Kosiborod said. “Our findings show that dapagliflozin is well-tolerated in patients hospitalized with COVID-19, with no new safety issues being observed. This should have implications for clinical practice given that our results do not support discontinuation of SGLT2 inhibitors in this setting, as long as patients are monitored.”
Overall, there were numerically fewer serious adverse events in patients receiving dapagliflozin versus placebo, researchers reported. Two non-severe cases of diabetic ketoacidosis were observed in the trial, both in the dapagliflozin group and in patients with prior history of Type 2 diabetes.
“Our study opens the door to asking additional questions,” Kosiborod said. “The idea for DARE-19 was quite unorthodox when we started—everyone was concentrating on antivirals and anti-inflammatory drugs, so it is fascinating to hypothesize that SGLT2 inhibitors may provide organ protection in acute illness. This should inform future clinical science and hopefully lead to further investigations.”
DARE-19 Study Details
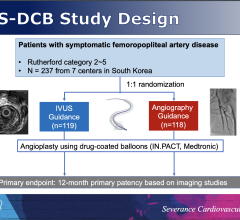
A total of 1,250 patients admitted with COVID-19 at 95 sites in the U.S., Brazil, Mexico, Argentina, India, Canada and the U.K. between April 2020 and January 2021 were included in the trial. Patients, who also had risk factors for developing serious complications, including high blood pressure, diabetes, atherosclerotic vascular disease, heart failure or chronic kidney disease, were randomized 1-to-1 to dapagliflozin (10 mg) or placebo once daily.
Patients started the treatment as soon as possible (and no later than four days following hospital admission) and continued the treatment for a total of 30 days, even if they were discharged from the hospital. Neither the patient nor the clinician or study personnel knew which treatment patients were receiving.
At 30 days, organ failure or death—one of the study’s primary endpoints—occurred in 11.2% of patients who were treated with dapagliflozin and 13.8% of patients treated with placebo. Altogether, 6.6% of patients in the dapagliflozin group died during study follow-up versus 8.6% in the placebo group.
Kosiborod said that for every component of organ failure or death endpoint—respiratory, cardiac, kidney failure or death from any cause—the results appeared to be directionally favorable for dapagliflozin as compared to placebo; however, because they did not reach statistical significance, further study is needed.
“Our study generates a hypothesis that dapagliflozin may offer organ protection in acutely ill patients who are hospitalized with COVID-19, but we were not able to prove this beyond a reasonable doubt because patient outcomes rapidly improved during the study period, making it much harder to accrue enough events and reach statistical certainty,” Kosiborod said.
Rapid improvements in the standard of care for patients hospitalized with COVID-19 between spring and summer of 2020 resulted in substantial declines in the number of patients with organ failure or death, he explained. For example, the mortality rate in patients hospitalized with COVID-19 in the U.S. decreased from approximately 25% to 5% between April and August of 2020.
The second primary endpoint of recovery, driven mostly by time to hospital discharge, was similar between patients taking dapagliflozin and placebo. Of importance, dapagliflozin was well-tolerated, with no new safety issues identified.
Additional data for 90-day follow up of these patients is still being evaluated. DARE-19 was funded by AstraZeneca.
Find links to more ACC 2021 late-breakers
Find more cardiology related COVID content
Related Dapagliflozin Content:
Dapagliflozin Reduces Heart Failure Worsening and Death in DAPA-HF Sub-analysis — ACC 2020 late-breaking study
FDA Clears Dapagliflozin to Reduce Heart Failure Hospitalizations
Dapagliflozin Meets All Endpoints to Treat Chronic Kidney Disease
Key Heart Failure Takeaways at AHA 2019
Farxiga Significantly Reduces Cardiovascular Death and Worsening of Heart Failure
Dapagliflozin Granted FDA Priority Review for Heart Failure With Reduced Ejection Fraction


 July 31, 2024
July 31, 2024