Staff member sets up an ECMO unit for a severely ill COVID-19 patient at Banner Health in Phoenix. A new study shows there is minimal safety risk in transporting patients who need ECMO to a hospital that can provide it as long as PPE requirements and other safety guidelines are met.
December 7, 2021 – Critically ill patients with COVID-19 can safely be transported for lifesaving extracorporeal membrane oxygenation (ECMO) therapy with no increased risk of transmitting COVID-19 transmission to ECMO transport team members following standard precautions. The was the findings of a study were published online in November in the ASAIO Journal, official journal of the American Society for Artificial Internal Organs.
In a large series of COVID-19 patients transported for ECMO, there were no cases of SARS‑CoV‑2 transmission to transport team members, according to the report by Jeffrey Javidfar, M.D., of Emory University, Atlanta, and colleagues.
"This pandemic and COVID-19 present a particular challenge to ECMO referral centers," Javidfar said. "But with thoughtful planning and meticulous execution, patients with acute respiratory distress syndrome secondary to COVID-19 can be remotely cannulated and then transported back to an ECMO center without posing an increased risk to the patient or the transport team."
Experience Supports Safety of ECMO Transport for COVID-19 Patients
ECMO is a life-sustaining therapy for selected critically ill patients. Like cardiopulmonary bypass during surgery, ECMO takes over the work of the heart and lung, but for a period of days or weeks, rather than just a few hours. Well-established for use in patients with other causes of acute respiratory distress, ECMO provides a chance for survival in a subgroup of patients with severe COVID-19.
Requiring specialized equipment and highly trained professionals, ECMO is mainly provided at large medical centers. Typically, ECMO teams travel to the location where the patient is hospitalized, initiate life support, and transport the patient back to the home hospital for ECMO care. But transporting COVID-19 patients might pose a risk of SARS-CoV2 transmission to ECMO transport team members, as well as a risk of complications and adverse effects to patients.
To assess the safety of ECMO transport, Javidfar and colleagues reviewed data on 101 adult COVID-19 patients (average age 46 years) transported to five different ECMO hospitals around the world. Most patients were transported by ground (ambulance), but 10 were transported by air. Average travel distance was 40 miles (36 miles by ground and 66 by air) and average transport time was 134 minutes.
Each multidisciplinary ECMO team included physicians, critical care nurses, an ECMO specialist or perfusionist, and a driver or pilot. Team members followed strict airborne contact precautions with eyewear (ACE) and personal protective equipment (PPE) protocols, including face shield or goggles, N95 or higher respirator or facemask, gloves, and an isolation gown.
“Special care was taken to not break ACE and PPE protocol from the time the team came into contact with the patient until they returned to their respective ECMO center,” the researchers write.
The evidence supported the safety of ECMO transport for COVID-19, both for patients and for mobile ECMO team members. None of the patients experienced transport-related complications such as pump failure or problems related to catheters placed for ECMO access.
"There were zero instances of transport team members contracting COVID-19 within 21 days after transport," Javidfar and colleagues write. That is consistent with previous studies showing that healthcare providers in critical care units are not at increased risk of SARS-CoV2 transmission, compared to the general population.
Patients remained on ECMO for an average of 22 days. Forty-four percent of patients survived to hospital discharge – a rate consistent with the growing experience with ECMO support for severe COVID-19.
The five hospitals contributing to the study were part of the COVID-19 Critical Care Consortium – a global alliance of healthcare professionals and researchers committed to using groundbreaking technology to identify the most effective treatments for the most critically ill COVID-19 patients.
"The COVID-19 Critical Care Consortium is a true global collaboration which has made this research possible," comments senior author Giles Peek, MD, of University of Florida, Gainesville. "Informing clinical practice for clinicians taking care of patients during the COVID-19 pandemic, the Consortium transcends institutional and national boundaries, as exemplified by this paper."
Read the article “Mobile Extracorporeal Membrane Oxygenation for COVID-19 Does Not Pose Extra Risk to Transport Team.“
Related COVID ECMO Content:
ECMO Increased Survival in Refractory Out-of-Hospital Cardiac Arrest
Similar Long-Term Outcomes With and Without ECMO for Mechanically Ventilated COVID-19 Patients
COVID Mother Reunited With Caregivers After Saving Her Live With ECMO
Abiomed Adds ECMO Cardiopulmonary Support to its Portfolio
FDA Allows Emergency Use of Impella for COVID-19 Patients on ECMO
VIDEO: ECMO Support Effective in Sickest COVID-19 Patients — Interview with Ryan Barbaro, M.D.,
FDA Approves ECMO to Treat COVID-19 Patients
VIDEO: COVID Survivor on ECMO in Hospital 152 Days Reunited With Clinicians Who Saved Her
ECMO Used to Treat Adult Respiratory Distress Syndrome Case
FDA Allows Emergency Use of Impella for COVID-19 Patients on ECMO
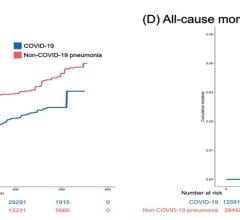
The Cardiovascular Impact of COVID-19
Reference:

 March 20, 2024
March 20, 2024