Sept. 9, 2025 — The American Venous Forum (AVF), International Society on Thrombosis and Haemostasis (ISTH), National Blood Clot Alliance (NBCA), Penumbra, the PERT Consortium and Society for Vascular Medicine (SVM) have come together to form the Get Out the Clot campaign. The groups have announced findings from a new survey assessing the current state of venous thromboembolism (VTE) care (blood clots). Get Out the Clot is a collaborative educational initiative to help identify gaps in patient care related to blood clot conditions, including standardizing care and expanding access to the latest innovations to improve patient outcomes.
"The 'Get Out the Clot' collaborative campaign unites the expertise and resources of leaders in the field of thrombosis and hemostasis to raise global awareness, foster innovation and ultimately improve outcomes for individuals affected by blood clot conditions," said ISTH President Pantep Angchaisuksiri, M.D.
The survey, which included nearly 270 healthcare professionals, both interventional physicians and non-interventional physicians caring for VTE patients, found that:
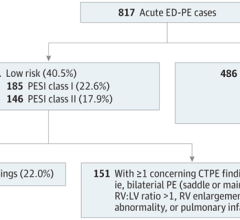
- Only 56% of interventional physicians surveyed believe their protocols provide clear direction based on pulmonary embolism (PE) risk beyond medical management and approaches vary, even for patients with the same risk profile. Further, only 39% of interventional physicians surveyed believe that their protocols provide clear direction for deep vein thrombosis (DVT) treatment beyond medical management, and approaches vary across patient types.
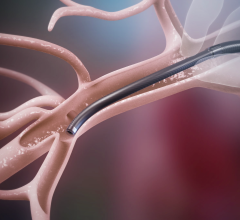
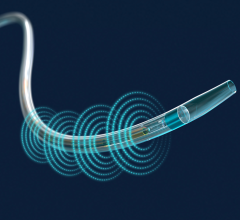
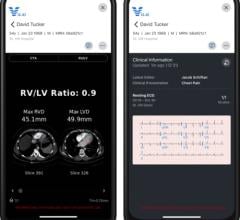
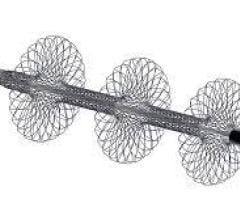
- Interventional physicians stated in the survey that they prefer newer treatment options such as mechanical thrombectomy, including computer assisted vacuum thrombectomy (CAVT), in combination with anticoagulation for 33% of their high risk and 37% of their intermediate-high risk PE patients. For intermediate-low and low-risk patients, most preferred anticoagulation alone.
- Nearly half of DVT patients are treated with anticoagulation alone. However, 71% of interventionalists surveyed state that they would like to see their hospital expand use of thrombectomy for DVT.
VTE affects up to 900,000 Americans annually, leading to approximately 100,000 deaths.1 VTE encompasses deep vein thrombosis (DVT, where a clot forms in a deep vein) and pulmonary embolism (PE, which is a clot that blocks the arteries in the lungs). Unfortunately, there are significant gaps and discrepancies in caring for these thrombus conditions, such as with PE, where there are often delays in care (up to 26% of cases in one study) and misdiagnosis (up to 53% of patients in one study).2,3
"The complexity of pulmonary embolism treatment cannot be overstated," said Herbert Aronow, M.D., MPH, Past President, Society for Vascular Medicine. "PE can be difficult to diagnose and, in many cases, if not treated quickly, can be life-threatening. Early identification is critical, and institutions must have a streamlined process to evaluate and treat patients."
Meeting Patient Needs
Collaboration and communication among physicians are crucial in determining the most effective care paths for patients, especially in complex conditions like VTE.
"Blood clots are often complex and the symptoms easily overlooked by both patients and healthcare providers, as symptoms can mimic other non-life-threatening medical conditions," said Leslie Lake, volunteer president of the National Blood Clot Alliance. "These survey results provide a vital opportunity to highlight critical information and identify appropriate support across the healthcare system to improve care and outcomes."
More than half of physicians surveyed report that they do not have a formal response team (e.g., a pulmonary embolism response team (PERT), or a venous thromboembolism response team) at their institution. Formal response teams streamline care through a collaborative multidisciplinary approach by engaging experts with the knowledge of and access to a broad spectrum of resources and procedures, potentially improving patient outcomes.
Additionally, only 35% of physicians surveyed perceive the ultimate treatment decision is made by consensus among specialties, showcasing that collaboration amongst physicians continues to be limited.
"The gaps and discrepancies in VTE care demonstrate why it is critical that health systems across the U.S. standardize care through collaboration among medical specialties," said Rachel Rosovsky, M.D., MPH, Immediate Past President, The PERT Consortium. "Studies have demonstrated that the formation of PERTs helps facilitate prompt diagnosis and the implementation of appropriate treatments in a judicious manner, leading to advancements in care, such as reducing the time to therapeutic anticoagulation – an essential aspect in PE care. Through PERTs and the adoption of efficient and effective practices, we can improve patient care and outcomes and ensure consistency of appropriate medical treatment across diverse patient populations."
The Next Phase
"Collaboration, innovation, and education will be the driving forces behind improving patient outcomes and providing consistent, high-quality care for all those affected by venous thromboembolism," said Mark D. Iafraiti, M.D., President Elect, the American Venous Forum. "By focusing on these priorities, we can create a more unified approach to VTE care, ensuring that patients receive timely, accurate diagnoses and the most effective care options available."
Nearly three-quarters (73%) of interventional physicians want to see expanded use of thrombectomy and CAVT at their hospitals for PE patients. These physicians believe the benefits of newer procedures, such as mechanical thrombectomy and CAVT, can improve patient outcomes, including minimizing ICU stays (57%) and rapidly improving hemodynamics (55%).
To achieve their goal of expanding use of thrombectomy in PE, the physicians surveyed believe their hospital would benefit from having more providers trained in these techniques.
"This survey sheds light on critical aspects of the current state of VTE care and the many opportunities to better align management protocols across the U.S. to work towards improving patient care," said James F. Benenati, M.D., FSIR, chief medical officer at Penumbra, the world's leading thrombectomy company. "At Penumbra, our focus is to continue to advance VTE care with technologies like CAVT, which has shown meaningful benefits on patient outcomes and the overall health systems."
To learn more about the survey and to help raise awareness of VTE symptoms and care options, visit www.GetOutTheClot.com.
1 Centers for Disease Control and Prevention. (2023, June). Impact of Blood Clots on the United States Infographic. National Center on Birth Defects and Developmental Disabilities (NCBDDD). https://www.cdc.gov/blood-clots/toolkit/impact-of-blood-clots.html?CDC_AAref_Val=https://www.cdc.gov/ncbddd/dvt/infographic-impact.html. Accessed July 9, 2024.
2 Chun Shing Kwok, Chun Wai Wong, Saul Lovatt, Phyo K Myint, Yoon K Loke, Misdiagnosis of pulmonary embolism and missed pulmonary embolism: A systematic review of the literature, Health Sciences Review, Volume 3, 2022, 100022, ISSN 2772-6320, https://doi.org/10.1016/j.hsr.2022.100022.
(https://www.sciencedirect.com/science/article/pii/S2772632022000113)
3 Hendriksen JM;Koster-van Ree M;Morgenstern MJ;Oudega R;Schutgens RE;Moons KG;Geersing GJ; (2017, March). Clinical characteristics associated with diagnostic delay of pulmonary embolism in primary care: A retrospective observational study. BMJ open. https://pubmed.ncbi.nlm.nih.gov/28279993/


 October 27, 2025
October 27, 2025