
Figure 1: Document radial artery readings along with the Barbeau test and mark the wrist for quick reference.
Staff education is a vital component for the successful transition to a predominantly transradial cardiac catheterization program. Educational efforts must extend beyond the cath lab. A successful program incorporates staff from the pre- and post-procedure units, telemetry unit, intensive care unit (ICU) and any other unit that routinely cares for cardiac catheterization patients. With this breadth of competency, care of these patients can be transferred from the cardiac cath lab to the other units, improving efficiency and leading to quicker turnaround.
Staff education involves both didactic and hands-on demonstration components. The staff must have an understanding of the vascular anatomy of the hand, complication recognition and thorough discharge instructions. Staff proficiency in assessment and removal of the hemostasis band is also a requirement.
In developing the transradial program at the Jesse Brown VA Medical Center in Chicago, we began a step-by-step process in the education of staff outside the cath lab. We began transradial cardiac catheterization procedures in May 2009. At that time in the United States, only 3 percent of heart caths were performed transradially. Due to the accumulating data indicating a decrease in bleeding complications, increase in patient satisfaction and a decrease in hospital stay time, we were encouraged to change our clinical practice. In the fall of 2009, once our lab had established standardized practices, we decided to extend the training out of the cath lab.
Pre-Procedure Considerations for Radial Access Patients
The ICU and telemetry staff were trained first, due to their technical skills and their familiarity with vascular access and arterial lines. The training was done at the change of shift to capture the greatest amount of staff and each unit was assigned a “super trainer.” To ensure understanding, a competency check list was made part of the staff’s mandatory training.
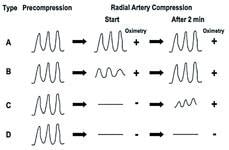
The Barbeau test[1] was taught to staff. This procedure is performed by placing the pulse oximetry on the patient’s index finger or thumb. The radial artery is occluded while the ulnar artery oximetry tracing and saturation numbers are noted. Release the radial artery and record the oximetric reading. If the waveform continues to be dampened two minutes after it is released, this is considered to be an abnormal test. You would repeat this step on the radial artery. This provides documentation of dual circulation to the hand. If there is poor waveform return, caution should be given to accessing the radial artery (Figure 2).
The characteristic of the radial artery is assessed on a 1 to 3 scale, 1 being weak and thready, 3 being pounding. Document radial artery readings along with the Barbeau test, and mark the wrist for quick reference (Figure 1). Also document whether the patient had any procedures or surgeries to the arm being utilized for access, such as an AV-fistula or prior radial artery harvest for bypass surgery. Always prepare the femoral area as a secondary access site.
Post-Procedure Consideration sin Radial Access
After the sheath removal, a hemostasis band may be applied to provide patent hemostasis. Patent hemostasis is the amount of pressure applied over the access site to prevent bleeding, while still providing blood flow to the distal extremities. The band we currently utilize is the TR Band (Terumo Interventional Systems). All hemostasis bands are placed over the access site and pressure is released over time until complete hemostasis is provided. We developed a flow sheet to assist staff members in other units. During the hemostasis period, capillary refill is checked along with pulse oximetry. Once the band is removed, the reverse Barbeau test is performed to assess radial artery patency. The reverse Barbeau involves compression of the ulnar artery and evaluation of the radial oximetric waveform. This documents the flow through the radial artery post-hemostasis.
After all patency checks have been completed, an Ace wrap or an arm board can be applied to prevent flexing at the wrist and assist in reminding the patient of the restrictions on the access site. Avoid blood pressures and blood draws from the procedural arm for 24 hours. You or the patient may remove the dressing in 24 hours and then wash with mild soap and water.
Discharge of Tranradial Patients
When giving discharge instructions to patients who are going home following a transradial procedure, instruct them to avoid excess moisture to the access site. Also, educate them on resisting the urge to submerge their hands in dishwater, bath tubs or other water sources for five days. Instruct them to avoid flexing at the wrist, such as hammering, playing tennis, or swinging objects. Also instruct the patient not to lift more than 5 pounds for 72 hours.
If bleeding or swelling should occur, apply manual pressure directly over the access site and report to the nearest hospital for evaluation. The patient must be taught to seek immediate medical attention if they experience loss of sensation, redness, swelling or discharge at the procedure site. For minor discomfort, the patient may take acetaminophen as prescribed, elevate the affected arm and apply an ice pack for comfort and swelling. Always provide the patient with a callback number, available 24 hours a day. Provide the patient with verbal and written post-procedure instructions.
Once the staff was trained to care for post-transradial cardiac catheterization, we instituted a same-day discharge program for elective percutaneous coronary intervention (PCI) patients. This was done to reduce the use of telemetry beds for post-PCI observation and eliminate an inpatient stay for an uncomplicated PCI patient. This led to cost savings, improved patient satisfaction and enhanced quality-of-care by allowing patients to return home on the same day of the procedure.
Criteria for such a program were published in an earlier edition of Diagnostic and Interventional Cardiology. However, post-procedure management of these patients is critical. Nursing and technical staff who care for post-PCI patient must have a very structured program to provide all the necessary care and education to these patients in a much shorter time frame.
Staff education is very important for a transradial catheterization program. It encompasses not just the cardiac cath lab staff, but also the other units that accept post-cath patients. When all units involved are knowledgeable about the care of transradial cardiac catheterization patients, continuity-of-care can be established, and patient safety and satisfaction can be increased.
Editor’s note: Stephanie Murray, RN, BSN, CCRN-CMC, works in the cath lab at the Jesse Brown VA Hospital in Chicago.
Related Transradial Access Content:
SCAI Updates Expert Consensus Statement on Best Practices for Transradial Access in January 2019
VIDEO: Trends in Radial Access for Percutaneous Coronary Interventions — Interview with Sunil Rao, M.D., and Prashant Kaul, M.D.
Patient Satisfaction and Complications of Transradial Catheterization
Radial Access Adoption in the United States
VIDEO: Update on U.S. Transradial Access Adoption With Sunil Rao at TCT 2015
Eight Tips to Make Radial Access Successful
Radial Access May Offer Cost Savings
VIDEO: Radial Access Recovery Lounge Mimics Cafe Atmosphere
The Economic Benefits of Transradial Access
Tips When Prepping for Radial Procedures


 November 14, 2025
November 14, 2025 









