February 7, 2008 - A Northwestern University Feinberg School of Medicine researcher has launched the first U.S. trial in which a purified form of subjects' own adult stem cells is transplanted into their leg muscles with severely blocked arteries to try to grow new small blood vessels and restore circulation in their legs.
The first two subjects in the 20-site national trial recently underwent the stem cell transplant process at Northwestern Memorial Hospital.
Severely blocked arteries in the leg and sharply diminished blood flow can result in wounds that don't heal, the breakdown of tissue and gangrene. This painful condition, called critical limb ischemia (CLI), results in the amputation of more than 100,000 limbs every year in the United States. It's a serious, emerging health problem that affects 1.4 million people. An estimated 15 percent of the population will have this disease by the time they reach age 70.
The Northwestern-led Phase I/IIa study—which will include 75 people with CLI around the country—targets patients who have exhausted all other medical options including angioplasty, stents and bypass surgery to repair blocked circulation in their legs.
"They're at the end of the therapeutic road and they're ultimately facing potential amputation," said Douglas W. Losordo, M.D., the Eileen M. Foell Professor of Heart Research at the Feinberg School and principal national investigator for the study. "This is hopefully a way to help them avoid that."
Dr. Losordo is director of the university's Feinberg Cardiovascular Research Institute and director of cardiovascular regenerative medicine at Northwestern Memorial Hospital.
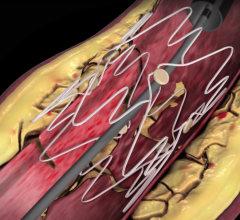
"The stem cells themselves can assemble into blood vessels," Dr. Losordo said. "They can also secrete growth factors that stimulate and recruit other stem cells to come into the tissue and help with the repair. It's an amazing biology we're trying to leverage in these folks."
He said preclinical studies transplanting stem cells into the limbs have shown this approach to be effective in mice and rats. "Based on that, we think it has a good chance of helping humans," Dr. Losordo noted.
"This is a dreadful disease in which the profession has failed to offer much in the way of relief for these patients," Dr. Losordo said. "We're hoping this will have some impact."
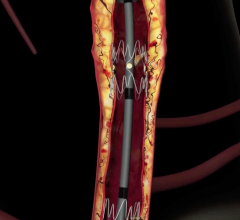
CLI is the result of advanced peripheral artery disease, which affects about 10 million people in the United States. In peripheral artery disease, people develop blockages in their arteries and vessels that slow or stop the blood flow to their legs. When they have pain at rest in their lower legs and wounds on their legs or feet that will not heal, they have CLI. If left untreated, CLI can result in a patient having toes, a foot, or even a leg amputated.
As CLI progresses, people begin to experience pain when they walk, then when just sitting. The worst pain occurs at night because blood flow is decreased when people lie down. Some have to sleep in chairs to aid the blood flow and lessen the pain.
"Peripheral artery disease is a big health problem," Dr. Losordo said. "An awareness of the impact of this disease on public health is emerging."
High blood pressure, high cholesterol, smoking, and diabetes all raise the risk of having the condition. But some people don't smoke, have diabetes or high blood pressure, and can still have blocked arteries in their legs, Dr. Losordo said.
For the randomized, double blind, placebo-controlled trial, Dr. Losordo uses the subject's own purified stem cells. The subject first takes a drug for five days to stimulate the release of his or her stem cells, called CD34 cells, from bone marrow. An intravenous line is then inserted into a subject's vein to collect blood through a machine that removes a population of blood cells that contains the CD34 stem cells. Dr. Losordo further selects and enriches the cells to select only CD34 cells.
Dr. Losordo's study is supported by Baxter Healthcare Corporation, which manufactures the Isolex 300i Magnetic Cell Selection System machine used in this investigational study. The Isolex 300i Magnetic Cell Selection System, which is approved for use in oncology patients, purifies the subject's stem cells to provide only the CD34 stem cells. Dr. Losordo is also a paid consultant to Baxter.
For more information: www.fcvri.northwestern.edu/index.html


 November 06, 2019
November 06, 2019